By Liz Manning
Reading this article and undertaking the learning activity is equivalent to 60 minutes of professional development.
This learning activity is relevant to the Nursing Council registered nurse competencies: 1.1, 1.4, 2.9, 4.3
Learning outcomes
Reading and reflecting on this article will enable you to:
- increase familiarity with the Code of Conduct standards for professional nursing conduct and behaviour
- practise applying the principles and standards of the Code
- raise awareness of the appropriate approach for health professionals towards professional boundaries, social media and electronic communications
- locate and review guidelines that underpin nursing practice.
Introduction
Three documents from the Nursing Council of New Zealand (NCNZ) provide a comprehensive guide to nursing professional conduct and behaviour in New Zealand.
The documents span all scopes of practice3,4,5 settings and specialties. Every nurse should be very familiar with these documents and copies of them should be easily accessible in all work settings. This article provides an overview of each document with useful tips and examples to prompt reflection. It does not cover everything OR replace the need to read the documents.
The Code of Conduct² is the primary document, with the two additional documents Guidelines: Professional Boundaries⁷ and Guidelines: Social Media and Electronic Communication⁸, providing extra information and guidance.
The Code of Conduct
“The Code is a set of standards defined by NCNZ describing the behaviour or conduct that nurses are expected to uphold. The Code provides guidance on appropriate behaviour for all nurses and can be used by health consumers, nurses, employers, NCNZ and other bodies to evaluate the behaviour of nurses²”.
The Code promotes four core values; respect, trust, partnership and integrity. These values are referred to throughout the eight principles and the 81 standards.
Code principles
- Respect the dignity and individuality of health consumers (10 standards).
2. Respect the cultural needs and values of health consumers (10 standards).
3. Work in partnership with health consumers to promote and protect their wellbeing (8 standards).
4. Maintain health consumer trust by providing safe and competent care (12 standards).
5. Respect health consumers’ privacy and confidentiality (8 standards).
6. Work respectfully with colleagues to best meet with health consumers’ needs (10 standards).
7. Act with integrity to justify health consumers’ trust (14 standards).
8. Maintain public trust and confidence in the nursing profession (9 standards).
The Code also contains guidance on: professional misconduct, escalating concerns, fitness to practise and public confidence.
| Code of Conduct Example 1: | “I’m worn out working two jobs; if it’s quiet I sleep through the night shift – I tell the HCA to wake me if anything major happens.” |
| Specific problems |
|
| Standards to consider | 4.2 Be readily accessible to health consumers and colleagues when you are on duty.
6.4 Your behaviour towards colleagues should always be respectful and not include dismissiveness, indifference, bullying, verbal abuse, harassment or discrimination. 6.8 When you delegate nursing activities to enrolled nurses or others, ensure they have the appropriate knowledge and skills, and know when to report findings and ask for assistance. 7.3 Act promptly if a health consumer’s safety is compromised. Other standards that may also apply here include 4.10 and 6.1. |
| Code of Conduct Example 2: | “I help my neighbour out by checking her husband’s clinical notes for his results as he never gets around to telling her; she says he doesn’t mind her knowing. He isn’t my patient but I can easily access his information.” |
| Specific problems |
|
| Standards to consider | 5.1 Protect the privacy of health consumers’ personal information.
5.2 Treat as confidential information gained in the course of the nurse-health consumer relationship and use it for professional purposes only. 5.6 Health records are stored securely and only accessed or removed for the purpose of providing care. 5.7 Health consumers’ personal or health information is accessed and disclosed only as necessary for providing care. Other standards that may also apply here include 5.5. |
Guidelines: Professional boundaries
Nurses must remember that within any professional relationship there is a significant power dynamic in play.
This dynamic – and the boundaries of professional practice – can be tested as nurses seek to support and empathise with patients and patients’ families. Patients and their families will often feel vulnerable and seek to increase a relationship with a nurse, feeling they can trust the nurse to have their best interests at heart.
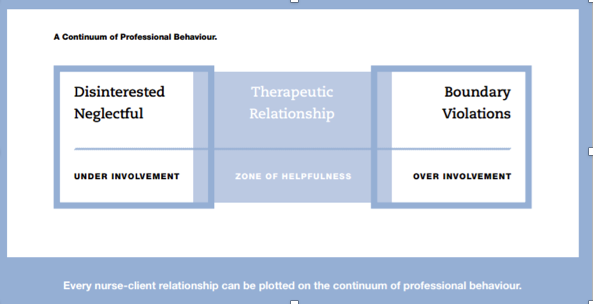
The professional boundaries document highlights the need for nurses to be responsible for maintaining a professional boundary in all aspects of the nurse-patient relationship, and gives examples that can occur across nursing. The balance required is illustrated using the ‘Continuum of Professional Behaviour’ diagram (see Figure 1).
The guidelines also contain clear and effective ‘questions for reflection’ on professional boundaries:
- Is the nurse doing something the health consumer needs to learn to do themselves?
- Whose needs are being met – the health consumer’s or the nurse’s?
- Will performing this activity cause confusion regarding the nurse’s role?
- Is the behaviour such that the nurses will feel comfortable with their colleagues knowing they had engaged in this activity or behaved in this way with a health consumer?
Key areas for nurses to be aware of are covered, including: caring for close friends or family; sexual relationships with patients or former patients or patients’ partners/family members; gifts, bequests, loans; financial transactions; power of attorney; and concluding professional relationships.
Boundary transgressions have resulted in some serious breaches and consequences. If you become aware of a colleague’s boundary transgression, the document provides advice on how to proceed.
| Professional boundaries Example 1: | “I house-sit for the family of a long-term patient. I had told them I don’t like my current flat and want to get away. They trust me and even pay me $50 a week for expenses.” |
| Specific problems |
|
| Standards to consider | 7.5 Act in ways that cannot be interpreted as, or do not result in, you gaining personal benefit from your nursing position.
7.6 Accepting gifts, favours or hospitality may compromise the professional relationship with a health consumer. Gifts of more than a token value could be interpreted as the nurse gaining personal benefit from his/her position, the nurse taking advantage of a vulnerable health consumer, an attempt to gain preferential treatment, or an indicator of a personal or emotional relationship. 7.13 Maintain a professional boundary between yourself and the health consumer and their partner and family, and other people nominated by the health consumer to be involved in their care. 8.8 Ensure you only claim benefits or remuneration for the time you were employed or provided nursing services. Other standards that may also apply include 7.8, 7.10, 7.11 and 7.12. |
Guidelines: Social media and electronic communication
Electronic communication is part of everyday life for most people, including nurses. Health professionals have a responsibility to take a more considered approach to what they communicate and to understand the consequences of what is sent in an email, text or posted online.
The social media guideline highlights specific areas related to breaching confidentiality and privacy, either intentionally or unintentionally, working respectfully with colleagues and employers, using professional language at all times, working with integrity and maintaining public trust and confidence in the nursing profession.
| Social media Example 1: | “If I post a photo or story about work on social media, I always keep the privacy setting to just my friends and I never use patient names.” |
| Specific problems |
|
| Standards to consider | 5.2 Treat as confidential information gained in the course of the nurse-health consumer relationship and use it for professional purposes only.
5.8 Maintain health consumers’ confidentiality and privacy by not discussing health consumers, or practice issues in public places including social media. Even when no names are used, a health consumer could be identified. 6.4 Your behaviour towards colleagues should always be respectful and not include dismissiveness, indifference, bullying, verbal abuse, harassment or discrimination. Do not discuss colleagues in public places or on social media. This caution applies to social networking sites e.g. Facebook, blogs, emails, Twitter and other electronic communication mediums. 8.1 Maintain a high standard of professional and personal behaviour. The same standards of conduct are expected when you use social media and electronic forms of communication. |
| Social media Example 2: | “I needed to place Mum in a rest home. I looked for the nurse manager of the nearest one online and his social media account was full of photos of his partying and bad language.” |
| Specific problems |
|
| Standard to consider | 8.1 Maintain a high standard of professional and personal behaviour. The same standards of conduct are expected when you use social media and electronic forms of communication. |
Remember!
- Employers, employees, staff, colleagues, patients and their family members may well check your online presence.
- Privacy settings do not prevent the sharing of information. Anything you send to another person can be copied and shared with others.
How do I use the documents if I’m concerned about a colleague?
Practice issues will often spread across a number of principles and standards. Check through the Code of Conduct and also refer, as required, to the two guideline documents.
- If you see a professional practice situation that concerns you to the degree that you think you need to refer your concerns, write it down.
- Refer to the Code and/or the social media and/or professional boundary documents.
- Review each principle and each standard to see where the issues you have identified fit.
- Note down the relevant standard(s).
- Follow your organisation’s professional practice reporting process.
Note: Check with your employer and employer policies in the first instance. If you then consider notifying the Nursing Council, ensure that what you have identified is a professional practice issue and not an employment issue.
In conclusion
These three documents, which are freely available on the NCNZ website, provide comprehensive guidance for professional nursing practice. Used alongside the relevant nursing competencies, they provide nurses, employers and the public with a clear framework for all aspects of professional nursing behaviour and conduct.
QUICK CODE CHALLENGESee if you can identify which principles and standards could be relevant to these three scenarios. |
|
| Challenge 1 | One of the clinic patients is Māori and she often requests that whānau come into the clinic room with her. It’s absolutely not appropriate in my view and makes me feel I’m being watched, so I’ve started saying no. |
| Challenge 2 | One of my colleagues shouts at residents who are hard of hearing. She really talks down to them and doesn’t bother explaining when she is doing something as she says it just takes ages. They don’t get a choice. |
| Challenge 3 | One nurse I work with was quite rough and demeaning to a patient in the emergency room and didn’t explain any of the care given. The patient was under police escort. I’ve seen this nurse behave this way many times with patients who are prisoners with guards or under police escort. |
Download the learning activity here >>
Useful tip
Refer to the below THREE documents if you are dealing with practice issues:
- Code of Conduct²
- Guidelines: Professional Boundaries⁷
- Guidelines: Social Media and Electronic⁸
The document may help you to identify or approach a situation. They can even provide helpful wording for framing feedback.The three documents, plus many more standards and guidelines are freely available to download from www.nursingcouncil.org.nz.
Recommended resources
- Health and Disability Commissioner (2009). Code of health and disability services. Consumers’ rights. Retrieved from www.hdc.org.nz/the-act–code/the-code-of-rights.
- The NCNZ’s Code of Conduct and Guidelines are freely available to download at www.nursingcouncil.org.nz/Nurses/Code-of-Conduct.
- The College of Nurses (NZ) website for Professional Support Guides on bullying and practice issues at www.nurse.org.nz/powerpoint-presentations.html.
- Worksafe NZ: Bullying Prevention Toolbox at www.worksafe.govt.nz/worksafe/toolshed/bullying-prevention-toolbox.
About the author
Liz Manning RN, BN, MPhil (Nursing), FCNA (NZ) is the director of Kynance Consulting and provides project management services, professional nursing supervision, coaching, mentorship and portfolio development support.
This article was peer reviewed by:
Cheryl Atherfold RN MHSc (Nurs) FCNA (NZ), who is an associate director of nursing practice and education at the Waikato District Health Board.
Erin Meads RN, BN, PGDipAdvNsg is the director of nursing for the Auckland-based primary health organisation ProCare.
References
- COLLEGE OF NURSES (NZ) Inc (2017). Professional Support Guides. Retrieved from
www.nurse.org.nz/powerpoint-presentations.html - NURSING COUNCIL OF NEW ZEALAND (2012). Code of Conduct. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2012). Competencies for Enrolled Nurses. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2017). Competencies for the nurse practitioner scope of practice. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2007). Competencies for Registered Nurses. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2011). Guideline: delegation of care by a registered nurse to a health care assistant. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2012). Guidelines: Professional Boundaries. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2012). Guidelines: Social Media and Electronic Communication. Wellington: Author.
- PRIVACY ACT (1993). Retrieved from
www.legislation.govt.nz/act/public/1993/0028/latest/DLM296639.html - WORKSAFE NEW ZEALAND (2017). Bullying Prevention Toolbox. Retrieved from
www.worksafe.govt.nz/worksafe/toolshed/bullying-prevention-toolbox.





















