To all of us grads, I say a huge congratulations for making it this far. Through the literal blood, sweat and tears, and other various bodily fluids, we’ve survived our first year of being RN’s – real nurses.
I’d say the new graduate year has been a year of rising. Rising to the occasion when you think you’re out of your depth, heart rates rising when your patient has chest pain (and now suddenly you’re the one who’s tachycardic, diaphoretic and nauseous), your preceptor’s eyebrows rising when you mess up something supposedly simple, and not to mention those rising cortisol levels when trying to get our assignments done in time while attempting to maintain that work-life balance (which I’m still not entirely sure exists).
Undoubtedly, our confidence has risen, our knowledge has increased. Our hearts rise when we receive smiles and thanks from patients and their families because they’re genuinely grateful for our care.
And of course, it has been a great year of learning. Learning how to master that clinical skill you always thought was kind of daunting as a student (and now you feel like a boss every time you do it), learning how to deal with all types of people, and learning about yourself too, like that you’ve got more resilience than you thought you did. And a bigger bladder.
And so we’ve come a long way, fellow graduates. While we recognise that we’ve reached a milestone, this is still the beginning of a journey. One that I am sure will contain opportunities for more rising and more learning.
So I’d like to say a huge thank you to those who have supported us in the journey so far: to our preceptors and senior colleagues, for their continual support and patience with us. And to our charge nurse managers, for the other kind of ‘patients’ and trusting us with them, we’re really grateful you hired us. Also to our lovely tutors – thank you so much for your guidance, advice and encouragement.
A shout-out to the PHC tutors, who had to drive all across town through traffic but still always arrived with big smiles, even to the Northland clinics (I mean, now that’s patience!). Thank you to our friends and families, for always being there through the ups and downs, and listening to our stories involving the other various bodily fluids – which I’m sure you really appreciated hearing over dinner.
And finally, thank you to my fellow graduates. For being there to share in our stresses about upcoming deadlines and ‘challenging’ patients, and for laughing through the hilarious and embarrassing moments – oh, the joys of nursing.
We’re always there for one other, so keep in touch, and keep supporting each other.
Aimee Lowe was the primary healthcare class representative for last year’s Waitemata DHB NETP (Nursing entry to practice) programme. She is a practice nurse at an Auckland GP clinic.
]]>On top of placement as undergraduates, since 2014, junior doctors have been required to take three-month stints in community-focused service, which is most often undertaken in general practice.
The research found that most general practices surveyed in the lower North Island and South Island were already involved in training doctors, nurses and other health care professionals. Most of the training GP clinics undertook was for medical trainees.
Two papers in today’s New Zealand Medical Journal have found 86 per cent of the practices surveyed in the lower North Island and South Island took at least one type of medical trainee, but in a comparable survey undertaken in northern New Zealand, the figure dropped to only 40 per cent.
The study of the lower North Island and South Island, led by Otago University researchers, found GPs needed more support to take more trainees as the current system was poorly co-ordinated.
Further, more were interested in taking junior doctors than undergraduate medical students.
The study of northern New Zealand, led by the University of Auckland, suggested that about 70 practices needed to start taking trainees by 2020 to meet demand, and that the proposed School of Rural Health will help with capacity issues.
“GPs and practice staff say there is little space at present for increasing numbers of trainees in practices,” Otago University researcher Dr Samantha Murton said of the clinics her team surveyed.
“In the future, under the current system, they say they would have to reduce the number of undergraduate trainees if they are going to take on more of those who are in a postgraduate or vocational training position [junior doctors and GP registrars],” she said.
It came at a time when there was increasing numbers of students in both medical schools, increasing numbers of postgraduate and vocational trainees and reducing numbers of GPs to supervise due to the ageing GP workforce.
“High quality primary care is an essential and pivotal part of New Zealand’s health system, and adequate training in primary care settings, for any health professional, is essential to support the present and future health of all New Zealanders.
“To resolve the training capacity issue, three key things are needed – robust and equitable co-ordination between all agencies involved in placing trainees, more training and support for teaching staff at practices, and for smaller practices, help to build additional consultation rooms,” co-author Professor Sue Pullon said.
“To achieve that we need a co-ordinated effort across the training system.”
Murton added: “The survey results suggest that there also needs to be support for teaching in different ways, which will help to make more room for quality teaching in general practice.”
]]>Shocked award winner Jess Tiplady flew back to Auckland this morning clutching an enormous bouquet of flowers, a beautiful trophy and an enormous certificate.
The 29-year-old, who became a primary health NP in April, was awarded NZNO Young Nurse of the Year 2017 at the organisation’s annual conference dinner at Te Papa last night.
The young NP is one of only four NPs under 35 and Tiplady (whose mother is Ngāi Te Rangi) is currently the youngest Māori nurse to have achieved NP status in New Zealand.
To become an NP by age 29, Tiplady has studied every year but one since first enrolling in nursing school. “It’s been a massive journey to get to here,” acknowledges Tiplady. She said she was shocked by her win, was very grateful, and felt the award was a reflection of how much others have helped her on her journey.
Kerri Nuku, NZNO’s kaiwhakahaere, said when presenting the award to Tiplady that she was a great example of a nurse making a positive contribution to health outcomes for New Zealand children living in poverty. “The impact on families living in overcrowded houses, with the associated infection, itch and discomfort of eczema, loss of sleep and potential for hospitalisation, is significant,” said Nuku.
Tiplady has worked for Manurewa’s Greenstone Family Clinic since graduating in 2001 with a conjoint degree in nursing and health sciences from the University of Auckland.
Primary health has been her passion from the start and she says becoming an NP followed on from that passion as it seemed to be a “really useful tool”.
Early on at her time at Greenstone, she looked at how she could make a difference and saw a niche in helping prevent eczema crises for children and their families. “We were seeing a lot of children with nasty skin infections, and not sleeping and some very distressed children and parents.”
Around five years ago she started providing a nurse-led clinic in eczema for children to provide a whole package of care to support parents and reduce the risk of eczema flare-ups and distress.
A year later she set up an asthma clinic for children with the aim of using the clinical guidelines for good asthma care in primary health to see whether a focused clinic could make a difference to hospital admissions for asthma.
Invitations to the asthma clinic was tied in with the annual reminder letter sent to all children on preventative inhalers that it was time for their free flu vaccine. “We altered our annual letter to say come in and have a 30-minute appointment with a nurse to have your annual asthma check-up,” said Tiplady. “It was kind of a ‘warrant of fitness’ going into winter.”
She said in 2015 its practice admission rates for children with asthma halved compared with previous years, but it was very difficult to prove whether that was due to the asthma clinic or other factors. “But I think what we have managed to do is establish a really good model of care where our children are getting what is considered to be the best practice package of care for their asthma.”
Tiplady said about 80-110 children under 16 are eligible for the asthma clinic each year. She said she and other nurses chased up children where there might be barriers to coming into the clinic or grabbed an opportunistic clinic appointment if the child came into the practice for another reason.
While the young NP really likes working with children and young people – and has a special interest in mental health – her scope is primary care and her day-to-day work involves seeing a cross-section of patients across the practice’s population.
She also offers fortnightly clinics in James Cook High School and Alfriston College, predominantly in sexual health.
Tiplady was a member of the first cohort of the pilot Nurse Practitioner Training Programme (NPTP) and was mentored by two GPs at the Greenstone clinic. She said a particular aspect of NPTP that was particularly helpful was having two protected clinic days a week to focus on transitioning from being a nurse to being an NP.
After so many years of study, she says the focus for the next year was consolidating her knowledge and establishing herself in her role as an NP. “And then looking at where else I can utilise those skills as an NP. The clinical role is most important to me but the NP hat also offers the opportunity to do research, teaching and mentoring so I will look at where I can contribute in those areas.”
The Young Nurse of the Award was set up to recognise and celebrate the work of nurses in the younger age group and to encourage younger nurses to demonstrate their commitment to the nursing profession. The winner is chosen for showing compassion or courage beyond what is expected in their role as a nurse and who has improved care or health outcomes for their patients through their commitment to care, leadership, research or quality.
Kerri Nuku said she also warmly congratulated runner-up Dana Smith from Dunedin Hospital general surgery. Smith was nominated by her colleagues for her work in the community with children with Crohn’s disease including volunteering at their annual camps,” said.
The judging panel consisted of a representative from Otago University Centre for Postgraduate Nursing Studies, previous years’ award winners, the Ministry of Health’s Chief Nursing Officer (or representative), and the NZNO president and kaiwhakahaere.
]]>
Nurses are the largest health professional group in a sector that takes a lion’s share of government funding.
Nurses deliver health care to young and old, rich and poor and the healthy to the dying, which gives them a unique insight into the state of our health system. Nurses have political views as diverse as any other section of the public, but share a common interest in wanting to do the best for their patients and clients.
This election the New Zealand Nurses Organisation’s election manifesto has also been supported and endorsed by the College of Nurses Aotearoa New Zealand.
The Nursing Matters manifesto sets out seven priorities for nursing and public health. Nursing Review gives a brief summary of how the released election policies to date of the five main political parties stack up against those seven priorities, plus mental health.
(See links to full health policies of the eight political parties in the running at bottom of article. The parties in that list and below are in alphabetical order.)
Nursing Matters Priorities
- A SUSTAINABLE, FULLY UTILISED NURSING WORKFORCE (N.B. We have included specific references to nursing in parties’ online policies here)
GREENS: Have a school nurse in every low decile school. Visits to nurses or doctors free for under-18s. Improve palliative care training for medical, nursing and allied health staff in hospitals, hospices and aged care facilities.
LABOUR: Extend nurse-led school-based health service. Fund an additional 100 Plunket and Tamariki Ora nurses.
NATIONAL: Introduce registered nurse prescribing. Nursing and doctor numbers employed in DHBs have increased by 6,900 in past nine years.
- INVESTMENT IN PUBLIC HEALTH
GREENS: Match increasing need for health services with increased funding.
LABOUR: An additional $8 billion investment in health over four years to meet inflation and demographic pressures and address current funding shortfalls.
MĀORI: Establish a new Māori and Pacific social investment fund managed by the Māori Pasifika Health Commissioning Unit.
NATIONAL: Health top funding priority, with Vote Health budget increased by $888 million for 2017-2018 to $16.8 billion. Increase number of elective surgeries to 200,000 a year by 2021. Social investment package.
NEW ZEALAND FIRST: Establish public health compact stipulating guaranteed minimum services. Adequately resource elective surgery and establish guaranteed maximum waiting times for surgical/specialist treatment.
- A PRIMARY HEALTH CARE APPROACH TO IMPROVING POPULATION HEALTH
GREENS: Review funding formula for primary care, specifically looking at high needs populations. Visits to nurses or doctors free for under-18s.
LABOUR: Cut GP fees by $10 a visit with $8 GP visits for community service cardholders. Review funding of primary care system. Review current funding model for residential aged care and update national baseline aged care standards.
MĀORI: Free annual and medical and dental visit for over-55s. Free GP visits and dental care for under-18s. Increase kaupapa Māori services. Increase mobile health clinics in rural communities. Explore the rollout of IMOKO nationwide. More Whānau Ora navigators.
NATIONAL: Cap the cost of GP visits to $18 for people with community services cards (estimated up to 600,000 extra New Zealanders could be eligible). Support family health hubs. Introduced Health Families NZ policy and combined phone helplines.
NEW ZEALAND FIRST: Review funding of primary health organisations. Introduce three annual GP visits for over-65s (SuperGold card). Fully fund palliative care services.
- ORANGA TAMARIKI – THE HEALTH AND WELLBEING OF CHILDREN AND YOUNG PERSONS
GREENS: Visits to nurses or doctors free for under-18s. Have a school nurse in every low decile school (see also mental health). Every baby gets baby pod at birth. Ensure only healthy food and drink sold at schools.
LABOUR: Extend nurse-led school-based health services to all public secondary schools. Extend paid parental leave from 18 weeks to 26 weeks. Support healthy eating and nutrition for children. Set child obesity reduction target and rollout Waikato’s Project Energize programme. Review Youth One Stop Shop funding (see also social and health equity priority).
MĀORI: Free GP visits and dental care for under-18s. Introduce mental health counsellors in all high schools. Subsidise power bills for those with rheumatic fever.
NATIONAL: New target of keeping children out of hospital for preventable conditions. Free GP visits and prescriptions for under-13s. Parents and newborns package including extending paid parental leave to 22 weeks. Ongoing policies include childhood obesity plan, Fruit in Schools and meeting B4 School Check and immunisation targets (see also social and health equity priority).
NEW ZEALAND FIRST: Nationwide health screening of all children under one-year (see also mental health). Support increasing paid maternity leave to 26 weeks and paid paternal leave of two weeks rising to four weeks.
- SAFE CLINICAL ENVIRONMENTS (see also investment in public health priority)
GREENS: Implement solutions to health workforce problems that have been jointly developed by health professionals.
LABOUR: Commit to building new hospital for Dunedin.
MĀORI: Increase in kaupapa Māori service.
NATIONAL: Invest in new hospitals in Christchurch, Greymouth, Dunedin. DHBs employing 6,900 more doctors and nurses than nine years ago. Establish a School of Rural Medicine.
NEW ZEALAND FIRST: Review number of district health boards (DHBs) and establish a ratio of practitioners to administrators.
- FAIR EMPLOYMENT
GREENS: Amend pay equity laws. Require all workplaces to measure and disclose pay gap between genders (see Labour below).
LABOUR: Pledged to scrap Pay Equity legislation currently in parliament. Make mental health workers a priority in pay equity negotiations. Labour and Greens Inquiry into Aged Care report notes pay equity settlement has created issues and funding concerns for sector, including loss of pay relativity for registered nurses.
MĀORI: No specific pay equity policy online. Introduce living wage for all workers.
NATIONAL: Introduced $2 billion pay equity settlement for 55,000 residential aged care and care workers. Legislation for pay equity framework currently before parliament.
NEW ZEALAND FIRST: Provide equality of funding for all family home carers. Review aged care sector funding – particularly rest home funding after pay equity.
- SOCIAL AND HEALTH EQUITY IN AOTEAROA
GREENS: Link benefits to fixed percentage of average wage, introduce universal child benefit (that can be capitalised for first home), tax free zone for first $10,000, look at benefit abatement for beneficiaries working part-time. Increase state housing units, expand social housing, more secure tenancy conditions and increase low-interest housing finance for low-income households.
LABOUR: Lift 100,000 children out of poverty by 2020. Legislate a child poverty reduction target. Implement a families package including Best Start scheme payments for children up to age of three for low and middle-income earners, continue with accommodation supplement increases and boost access to Working for Family payments. Increase minimum wage to $16.50 an hour and promote Living Wage. Stop sale of state houses and build more. Pass Healthy Homes Guarantee Bill to ensure rental properties warm and dry. Build 100,000 more affordable houses over 10 years. Implement rental reforms. Change Public Finance Act so Budget reports on reducing child poverty
MĀORI: Cost of living adjustment to all benefits. Introduce living wage. Housing policy includes developing National Housing Strategy, improve renters rights, enforce compulsory rental home warrant of fitness, provide low interest housing loans and introduce options for ‘rent to buy’.
NATIONAL: Family Incomes package from next year will shift tax thresholds for low income families, lifting Family Tax Credit up to age 18 and increasing accommodation supplement rates next year. PM Bill English says this will lift 50,000 children out of poverty and he pledges to bring another 50,000 children out of poverty by 2020 if re-elected. Increase social housing available from 66,400 to $72,000 over three years. Announced plan to build 34,000 new houses in Auckland in next 10 years. Budget had $20 million over four years for more emergency and transitional housing, expansion of Housing First programme for homeless and extending Warm and Dry upgrades of social housing. Would double HomeStart grants for first homebuyers.
NEW ZEALAND FIRST: Raise minimum wage to $20 an hour over next three years. Greater scrutiny of the benefit system, adjustment benefits and abatement levels. Remove secondary tax. Introduce flexible state support for grandparents raising grandchildren.
- MENTAL HEALTH
GREENS: Free counselling for all New Zealanders under 25 and increase youth mental health funding by $100 million a year. Support an independent inquiry into mental health
LABOUR: Initiate review of mental health and addiction services in first 100 days to identify gaps in services. Two-year pilot of basing primary mental health teams at eight primary health centre sites in high needs areas to offer early intervention and continuing care. Teams led by ‘doctors or other medical professionals’.
MĀORI: Expand Rangatahi Suicide Prevention Strategy. Increase kaupapa Māori mental health and addiction services. Support an independent inquiry into mental health. Reduce tobacco supply and subsidise e-cigarettes. Eliminate synthetic cannabis. Increase respite care beds for P-addicts.
NATIONAL: Increased funding announced in Budget including $100 million over four years for 17 social investment initiatives and pilots. Mental health funding services increased from $1.1 billion to $1.4 billion. Moving to emphasis on mental wellness, resilience and new ways of accessing services.
NEW ZEALAND FIRST: Re-establish Mental Health Commission. Commit to a suicide reduction target. Support an independent inquiry into mental health. Increase mental health service options and beds especially around child and youth mental health services.
HEALTH POLICY LINKS
ACT: http://act.org.nz/health/
Greens: https://www.greens.org.nz/page/health-policy
Labour: http://www.labour.org.nz/health
Māori: http://www.maoriparty.org/health_policy_2017
National: https://www.national.org.nz/health
New Zealand First: http://www.nzfirst.org.nz/health
The Opportunities Party: http://www.top.org.nz/top15
United Future http://unitedfuture.org.nz/our-policies/
]]>
Roberta Kaio, who is of Ngāti Kahu ki Whangaroa and Ngāpuhi Nui Tonu descent, says she will use the scholarship to complete her Master of Nursing at the University of Auckland.
She currently works as the primary mental health co-ordinator for Kaitaia-based Te Hiku Hauora’s mobile nursing team, which serves the Far North.
Kaio, who started nursing training later in life, said she was very grateful for the scholarship and the chance to continue her postgraduate study, after already gaining postgraduate diplomas in health management and nursing.
“I remember the days as a single mother with two children, knowing I had to do something better for myself and for my children,” says Kaio. “I became passionate about supporting people with mental health issues and those who experience abuse.”
After 22 years in Auckland, the mental health nurse moved to Ahipara with her husband and children to reconnect with whānau and the community. “We now have a better life balance, with time for fishing, being outdoors gathering kai, and time on the beach together.”
Her first job in the Far North was further south working for the Ngāti Hine Health Trust as the clinical lead and acting team leader for Mental Health and Alcohol and Addiction Residential and Community Services, until a position became available serving the Far North.
“I spend a lot of time travelling to clients across the rural Far North; however, I get a great deal of satisfaction seeing the work that I do make a difference to the community, and I enjoy being part of people’s journey in a positive way.”
“Community-based rural health services are essential for people living in remote areas,” says Fiona Gower, RWNZ National President. “It is heartening that health professionals like Roberta are passionate about working in regions such as the Far North, and undertaking further study to improve professional knowledge and experience for the provision of quality rural health services.”
Kaio’s most recent job in Auckland was as service manager for Mobile Community, Adult, Youth and Maternal Respite Services for Affinity NGO Services. She has also worked for Māori Community Mental Health Services for several district health boards in Auckland and at the Mason Clinic.
]]>His comments follow a Herald investigation that found that preventable, housing-related illnesses such as pneumonia and bronchiolitis killed more kids than car crashes or drownings.
On top of the deaths, 30,000 hospitalisations a year are associated with unhealthy homes.
The majority of those were from respiratory diseases including the third-world condition bronchiectasis, where babies’ lungs are scarred for life.
Coleman said the National government had set a target to reduce avoidable hospitalisations, which included earlier interventions and best treatment of respiratory illness.
He said: “No doubt that this is an unacceptable statistic and there is a lot more work to be done.”
Coleman said the government had already made child health a priority with free GP visits and prescriptions for under 13s, insulating 300,000 homes, setting the first rheumatic fever reduction target, and dramatically increasing immunisation rates.
The diseases included in the Herald’s investigation did not include vaccine-preventable conditions.
It detailed how the rheumatic fever target wasn’t met, including how a Healthy Housing Initiative was unable to rehome 75 per cent of families at risk of rheumatic fever due to a lack of housing supply.
Labour leader Jacinda Ardern called the situation “deeply saddening”.
“This is what this election should be about. This is what we should be debating – do we have a tolerance for kids dying because our houses are in such a bad state? Do we tolerate this?” said Ardern.
“The idea a kid dies because they’re cold is just appalling in a place like New Zealand.”
If elected the party would address unhealthy homes in its first 100 days, by introducing the party’s Healthy Housing Bill, mandating high insulation standards and requiring rentals to be warm, dry and healthy.
It would also fund universal $2,000 insulation grants, offer a $700 winter energy payment and build more state houses.
The Green Party’s social housing spokeswoman Marama Davidson said the deaths were an “absolute farce and an absolute scandal”.
Davidson said the Greens would bring in a comprehensive Warrant of Fitness for houses to make sure all properties, not just rentals, were warm, dry and safe.
“We want people to be able to heat their houses sufficiently. We know lots of people can’t afford adequate heating at the moment.”
She said the Greens would also boost a government insulation programme back to former levels.
A range of organisations condemned the high hospitalisation rates yesterday, including the Asthma and Respiratory Foundation and health bodies.
Plunket’s Chief Executive Amanda Malu said Plunket nurses regularly see babies living in “bone cold”, damp, overcrowded houses – some with no curtains or with holes in the floor.
“This is a systemic issue and policies are needed to increase access to quality houses for families.”
]]>The module has been developed by a team of researchers at the University of Otago, Wellington, to provide ‘realistic and practical guidance’ for nurses and doctors working with interpreters, particularly in primary health care. It was a response to the growing number of new New Zealanders – both migrants and refugees – with limited proficiency in English and builds on research carried out since 2009 into using interpreters in primary care.
One of the module developers, Jo Hilder, said professional interpreting services were increasingly available but were still under-utilised and it was hoped the learning module would help both practising clinicians and students to be more aware and confident of working with interpreters.
The module features a toolkit of flowcharts and tables that highlight what to consider when making decisions on the best approach for a given situation and the pros and cons of the different interpreting options, including using family. Hilder said they used authentic video footage, with the full consent of all involved, of real doctors and nurses working with patients and interpreters.
The learning package covers a range of topics, including practice advice on seating arrangements and the extra care and skill required if nurses and doctors are considering using patients’ family members as an interpreter option. The focus of the module is on spoken language, but it also provides some information on interpreting NZ Sign Language for deaf patients. The authors also point out that the module is focused on primary health care and there would be slightly different needs for other forms of care, such as mental health care, in-patient care and emergency department care.
The resource is available online here.
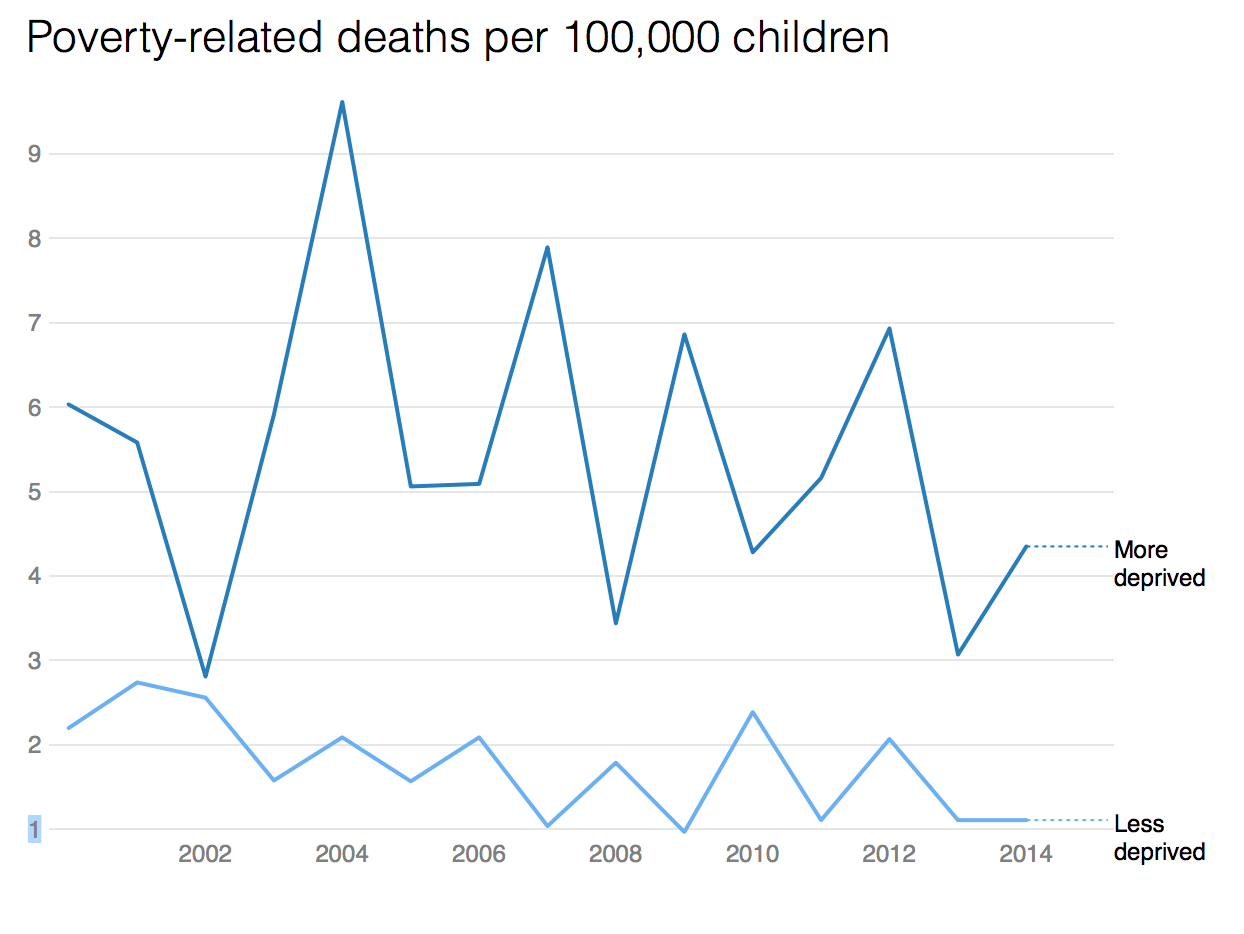
]]>An average 20 children die and 30,000 are hospitalised every year from preventable, housing-related diseases like asthma, pneumonia and bronchiolitis, health statistics show.
(For related full New Zealand Herald investigation article including frustrations with funding of nurse-led healthy housing initiatives click here)
Poor areas suffer the most – suburbs like Auckland’s Pt England and parts of Glen Eden – because of high deprivation and low incomes, lots of rental housing and fewer Europeans.
The illnesses peak in winter. They kill more children than either car crashes or drownings, which claim an average 10 lives a year each.
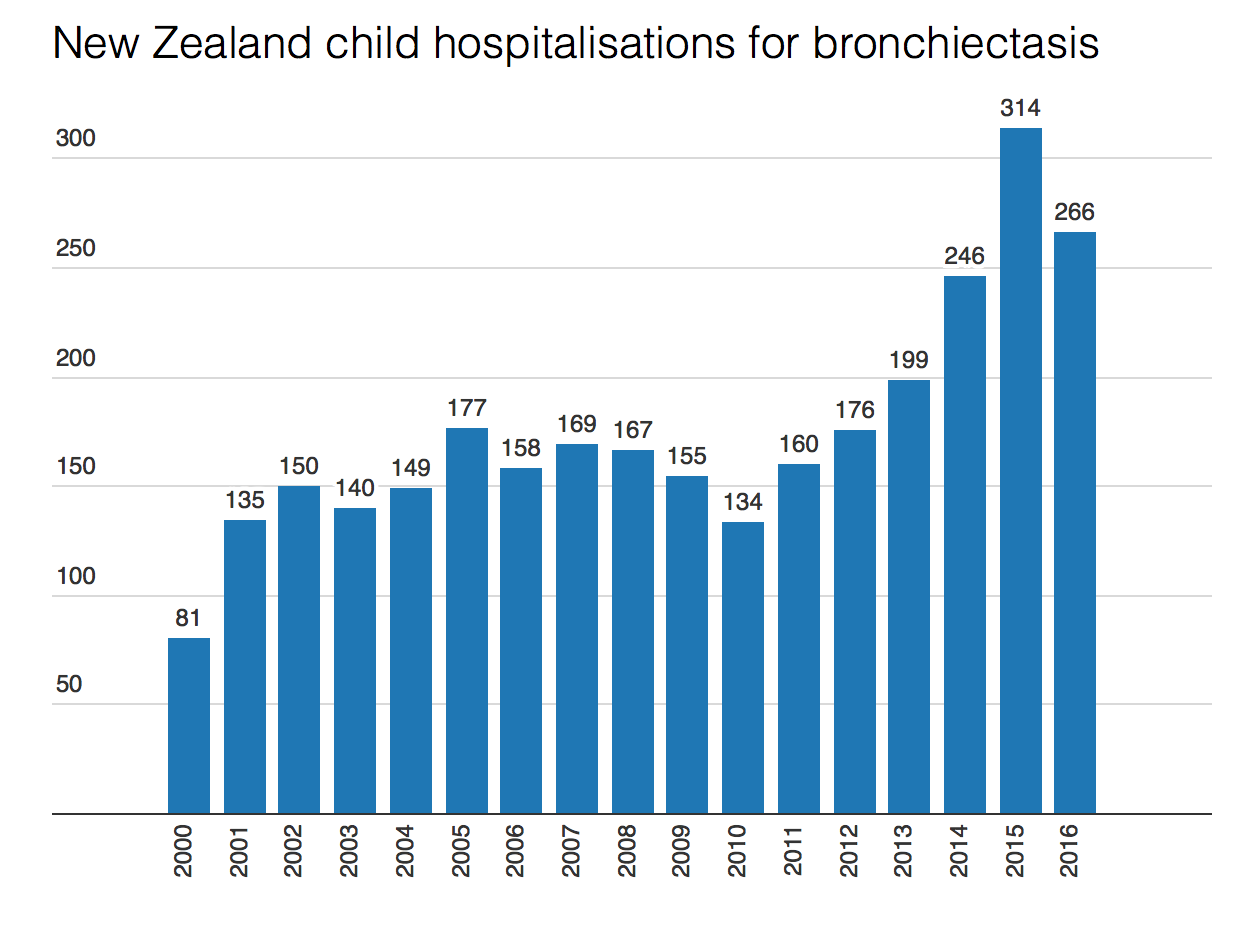
Health data shows the hospitalisation numbers are climbing. Respiratory conditions in particular – like bronchiolitis and asthma – are causing more hospitalisations each year, with the most severe, such as a “third world” disease named bronchiectasis, irreparably damaging babies’ lungs.
“We have waves of kids coming in the minute it gets cold,” says paediatrician Cass Byrnes.
“We try to delay discharges but the wards are packed. The problem is, the kids just can’t get symptom-free – they go home with antibiotics to the same environment that causes the problem.”
Doctors are calling for an urgent change in housing, saying the combination of child poverty and “shocking” housing conditions have been normalised.
“Inequities in health outcomes will persist unless such stark social inequities are urgently addressed,” the Royal Australasian College of Physicians said.
Interventions by the government have not met demand, doctors said.
Otago University’s Dr Nevil Pierse, deputy director of the housing research unit He Kainga Oranga, said criteria for the Healthy Housing Initiative – initially aimed only at families at risk of rheumatic fever – were too strict and many families were missing out.
The initiative missed children suffering from common conditions like asthma and skin infections, and was also limited to the poorest families.
Nurses were funded to assess houses, but then the money dried up, and families relied on charity or their landlord to provide the required provisions such as curtains, bedding, or insulation.
Data shows that of the 5500 families referred so far, 4020 were assessed.
An average 60 per cent of those who needed them received curtains or floor coverings, but only 34 per cent of recommended insulation was installed. Just 25 per cent of families nominated for new houses were able to move, because of the housing crisis.
“Basically, they’re doing the right thing but they’re doing it too cheaply. There’s not enough kids, not enough criteria, not enough help,” Pierse said.
“It’s just ridiculous – if there was a new pill they would spend the money. If there was a pill as effective as good quality housing the health sector would spend the money so why don’t they spend it on this?”
Those working in the field said one of the biggest barriers to progressing interventions like insulation were landlords – who had to pay half the cost.
Ministry of Health spokesperson Dr Stewart Jessamine said the environment in which the interventions worked was “complex and challenging” as staff had to liaise with multiple agencies.
He said sometimes it was difficult to contact the families as well as landlords. Landlords were able to decline interventions, he said.
Despite the difficulties, the ministry considered the project a success and many more thousands of families were expected to benefit in the coming years, particularly with “vulnerable” families now included in risk criteria.
Health minister Jonathan Coleman said the housing interventions would be continued as part of the government’s new target of reducing avoidable child hospitalisations by 25 per cent in five years.
It will also “work in partnership” with other agencies to reduce housing-related health conditions. He did not describe what that would entail.
‘Bronchiectasis: It’s completely terrifying’
When Niki Te Puni said the name of her daughter’s disease over the phone, her mum went silent at the other end.
“That’s when I knew it was bad,” Te Puni says. “Mum’s a paediatric nurse and she knew exactly what it was. I couldn’t even pronounce it.”
Te Puni’s daughter Kierra, then just 2 years old, had been diagnosed with bronchiectasis, an irreversible, life-threatening lung disease caused by repeated chest infections.
Kierra, now 5, was among 99 children to be diagnosed with the condition that year. Rates have kept climbing since, and now 300 New Zealand kids have a disease that should be confined to geriatrics.
“It’s a third-world disease, the kind of thing that if you were going to see it, the patients would be in their 80s,” says Byrnes, from Starship children’s hospital.
“Internationally people are astonished at the numbers we have here. It’s completely terrifying.”
Bronchiectasis is caused by scarring in the lungs, which allows mucus to build up and leads to ongoing infections. It’s linked to cold housing, and other unhealthy conditions like dampness, or inside smoking. It can be fatal.
When Kierra was diagnosed, a young girl the family knew in Whangarei had just died from it.
“It was heart-wrenching,” Te Puni says. “And it’s exhausting. We are constantly at the doctors, constantly making Kierra wear a jacket, a beanie, shoes. Even though she loves shorts.”
They also replaced a gas heater with a heat pump, to warm their high-ceilinged older home.
Te Puni says she wants to raise awareness about the disease, to let others know it’s not normal for kids to be coughing all the time, or to have a snotty nose.
The family are determined to give Kierra as normal a life as possible. Sometimes it’s not easy: she gets bored of her breathing exercises and just wants to be like the other kids. It can be a struggle not knowing if her condition will worsen in time.
“I have no idea what’s ahead for us,” Te Puni says. ” What’s in our future next week or next year. Sometimes we feel like the only ones going through it.”
]]>The plan was to run a contestable business case process with currently two proposals in the running – the initial joint Waikato University and Waikato District Health Board proposal and the joint Otago and Auckland medical schools proposal.
Professor Jenny Carryer, executive director of the College of Nurses, said the Government committing to a new rural medical school with the specific intent of producing 60 additional doctors a year for rural health was “extremely disappointing”. She said training more doctors flies in the face of evidence and advice and a more cost-effective solution was to train more nurse practitioners who could deliver the same scope of service as GPs.
Dalton Kelly, the chief executive of the New Zealand Rural General Practice Network (RGPN), said establishing a new rural school of medicine would be “very, very good news” as the initiative would contribute “hugely’’ to ensuring rural New Zealanders had the best health services available. But RGPN wanted to ensure the new school was multi-disciplinary, and not just for doctors. Kelly said it wanted the school to be for nurses, pharmacists, midwives, physios and for all the health disciplines needed to ensure “the first-class delivery” of health services in rural New Zealand.
Carryer said New Zealand had tried for many years without success to provide GPs for rural areas and had spent millions of dollars on an endless rotation of locums. “Medical graduates move towards busy urban areas and specialist positions with higher incomes and status,” she said. “Nurses are resident in rural areas and evidence shows they remain there after becoming nurse practitioners”.
Professor Neil Quigley, the University of Waikato’s Vice-Chancellor, said the university was heartened that National’s election promise showed its proposal last year for a Waikato Graduate Entry Medical School had been recognised and acknowledged. He said that the international research in medical education indicated that the only way to address the rural primary health care shortage and “looming crisis” was through the creation of a third medical school with a dedicated graduate-entry programme focused on community-engaged medical education outside the main centres.
In March the University of Otago and University of Auckland medical schools, in association with the Royal New Zealand College of General Practitioners (RNZCGP) and the New Zealand Rural General Practice Network (NZRGPN), announced they were investigating creating a new National School of Rural Health as a joint initiative. A key part of the proposal was to have a rural component for all health professional students by building an “interprofessional” faculty with its own leadership, based at up to 20 sites located in rural communities across New Zealand, which the partners believed had the potential to begin to address the country’s chronic shortage of rural health professionals.
Goldsmith’s announcement did not mention nursing or allied health professionals but said the business case process for the new school would ensure it met the needs of rural New Zealand. Also that the Government was committed to growing the medical workforce to meet the needs of a growing and ageing population.
Carryer said producing an NP from a year 1 nursing degree student through to completion of a master’s cost about $120,000, compared with about $600,000 to train a GP. “We cannot afford to pour more money into a direction, which is not supported by evidence or good sense.”
(See earlier opinion piece by Carryer: Train more GPs, not NPs and one GP’s response.)
]]>
Labour said the remaining New Zealanders who are not on low incomes will still see their doctor visit fees drop by about $10 if their GP practice signs up.
Labour leader Jacinda Ardern announced the policy at the party’s Pacific launch in Mangere on Saturday.
National last week announced a policy to extend $18 doctor visits to another 600,000 low-income New Zealanders.
Ardern said that didn’t go far enough, and under Labour those subsidised visits would drop to $8.
“This will apply to people enrolled in both Very Low Cost Access practices and other practices.”
Labour said Kiwis who are on the Very Low Cost Access scheme or are Community Service Card holders will have their maximum fee cut from $18 to $8, and costs for teenagers will drop from $12 to $2.
Under-13s will remain free.
As part of the policy, the Community Services Card will be extended to another 350,000 New Zealanders.
Adults and teenagers who are not on the low-cost scheme will get a $10 reduction in their fee if their GP practice chooses to take up the extra funding offer. Labour said this would reduce the average fee from $42 to $32.
Ardern said funding for the policy would come from the $8 billion of increased health funding pledged by Labour over the next four years.
“GP practices will also get a further $46 million over and above the funding to reduce fees, a five per cent increase on current funding… Labour will also invest $30 million over three years to boost the number of GP training places to 300 a year.
“This initiative will cut fees for New Zealanders while we undertake a full review of the primary care system aimed at better targeting subsidies, ensuring practices’ financial sustainability and reducing other barriers to access. This review will keep zero fees for under-13s and look to further lower fees for others,” Ardern said.
Labour said its GP policy would cost $259 million per year.
The announcement was met with cheers by crowds of hundreds at the Mangere town centre. Pacifika children were more likely to develop rheumatic fever, which Ardern described as a national shame.
“We know that will make a huge, huge difference,” Ardern told crowds.
National Party campaign chair Steven Joyce said Labour’s policy was a copy of National’s announcement earlier this week, with a $10 universal subsidy tacked on.
“That’s the level of thought they have put into it. Targeting low-income New Zealanders is a good idea, which is why we announced it. But for every other New Zealander it’s a poor exchange.
“If Labour committed to National’s Family Incomes Package, families would put some of the money towards a doctor’s visit one week, and something else they need the next week. Why can’t they trust people to make more of their own decisions?”
GP fees – how Labour says they will change under its policy
Very Low Cost Access practices:
• 13-17-year-olds: from $12 to $2
• Adults: from $18 to $8
Other practices that sign up to the extra funding:
• 13-17-year-olds: from $30 to $20
• Adult: from $42 to $32