Parliament is today to sit under urgency to debate the Families Package (Income Tax and Benefits) Bill. The bill would bring into effect the package announced yesterday that aims to bring 88,000 children out of poverty through a combination of higher Accommodation Supplement changes, more generous Working for Families scheme, a “Best Start” payment for parents of young babies, and a “Winter Warmer” grant for beneficiaries and superannuitants.
Memo Musa, chief executive of the New Zealand Nurses Organisation said nurses had seen an increase of child illness due to poverty and damp, poor living conditions so welcomed the package’s increases – particularly the Winter Energy Payment.
“Increasing money directly to families may well be the difference to having to access a health professional for some illnesses because affording healthier food or extra medicines and adequate, quality clothing can help to prevent illness.”
“Kiwi kids suffering from preventable illnesses are often linked directly to living in poverty. Increasing minimum wage, reduced health check fees, increase in parental leave and the Family Package are all key steps to reducing illness that nurses are saddened to see on a daily basis,” Memo Musa said.
Radha Balakrishnan, Plunket’s chief strategy and performance officer, said with Plunket nurses seeing 9 out of 10 babies born in New Zealand they see first-hand the impact of poverty and poor housing on child health – “particularly on Māori and Pacific communities who bear the brunt of this burden on our children”.
“We welcome Government action to level the playing field, and address the inequity of health and wellbeing outcomes among New Zealand’s tamariki and whanau,” she said. “We will be looking for further action to tackle systemic issues that are having an unacceptable impact on children’s health.”
Paula Bennet, National’s spokesperson for children, described the Government’s package as bluster and said National’s Families Income package was projected to lift 50,000 children out of poverty on April 1 2018 and it had committed to a further package in 2020 that would have had a similar effect.
“Labour has reverted to type by throwing billions of dollars at poorly targeted hand-outs, including over $3000 baby bonuses that go to everyone, irrespective of whether they need it or not, said Bennett. “During our term in Government, the number of kids in material hardship fell by nearly 40 per cent to 135,000 in 2016.
Andrew Becroft, the Children’s Commissioner, described the package as “really positive steps” as raising family incomes, enabling warmer and more support for the first year of a child’s life would contribute to improving outcomes for children.
He said the office would be monitoring whether the projected aim of raising 88,000 children out of poverty by 2021 was successful through its ongoing Child Poverty Monitor (which has just received continued funding from the JR McKenzie Trust for a further three years). “We look forward to seeing the significant improvements in the wellbeing of children that this package promises.”
Associate Professor Susan St John, the economics’ spokesperson for the Child Poverty Action Group, welcomed the package as a “long overdue response to the disastrous child poverty experienced since the 1990s”.
“But there are still some complex issues and CPAG would welcome working with Government on ways to simplify and extend the package,” said St John. “We would especially urge the Government to help the very worst-off children who are still excluded from the full package.”
]]>
The conference follows a week of ongoing media headlines over concerns about district health board deficits, understaffing and delayed surgery, alongside speculation on which way Winston Peters will swing when coalition talks get underway.
During that week the New Zealand Medical Association also released its Health as an investment position statement that calls for a public debate regarding the level of health funding needed to fulfill the original aims of universal access to comprehensive public health care.
“Nearly 80 years ago New Zealand led the world when we established a public health care system that made health a universal and fundamental right – it’s time our political leaders invest in that promise,” said NZMA chair Dr Kate Baddock.
She said health spending must not be seen as a drain on the economy but as a boost to the economy that improves the lives of New Zealanders. Also required was a commitment to address the social determinants of health such as education, housing and poverty.
Last week NZNO associate professional services manager Hilary Graham-Smith endorsed that by calling for the new government to “get people out of living in cars and damp garages and ensure tamariki are physically and sexually safe”.
“This is not a 100-day aim, this is now, immediately,” Graham-Smith said.
Lindbergh said the PHA endorsed the NZME statement. “As long as government fails to address the underlying causes of illness – poverty, inadequate housing, uncertain work, and educational failure, the health system only will continue to require greater investment,” he said.
He added that cost saving – as the population grew, aged and became more diverse – simply resulted on greater pressure on health services which were now “way beyond reducing costs through so-called ‘efficiences'”.
The senior doctors union, the Association of Salaried Medical Specialists (ASMS), also welcomed the NZMA statement, saying the next government should ensure that spending on our public health service should be seen as an economic and social investment.
“This statement draws attention to international research that indicates other countries are achieving a return on investment of nearly $5 for every $1 of government spending on health,” said Ian Powell, executive director of ASMS.
]]>
Former Counties Manukau midwife Danielle Hart-Murray’s Facebook post – describing the poor health of many children and the terrible living conditions of some of her clients, including some pregnant due to incest – went viral earlier this month (see post detail below). Her former employer, Counties Manukau DHB, last week asked Hart-Murray to remove the post out of concern that it breached patient privacy. A DHB spokesperson told the New Zealand Herald that staff members had recognised the cases referred to in the post and acted quickly to have the post removed.
Associate Professional Services Manager Hilary Graham-Smith said NZNO was very concerned about the issues expressed by the midwife, who had “bravely shared” her distress about housing, poverty and the resulting infant and child illness. She said the impact of poor housing and poverty and limited access to good health care was a national shame.
“The new government must get people out of living in cars and damp garages and ensure tamariki are physically and sexually safe. This is not a 100-day aim, this is now, immediately,” Graham-Smith said.
She said preventable diseases such as skin infections, rickets and respiratory diseases should not be a feature for any child growing up in Aotearoa.
“Incest resulting in mental and physical trauma and unwanted pregnancies for young women is an indictment on the conditions in which some people live because of poverty, leading to unwanted bed sharing, substance abuse and inadequate accommodation,” said Graham-Smith.
“We are speaking out in support of this midwife to let New Zealanders know the mental health and general health risks when people live in cars and garages and in squalor and call on the next government to urgently turn this shame around.
“We agree with and support Women’s Health Action maternal and child health manager Isis McKay that it is important for health professionals to speak out and highlight these terrible situations and the physical and mental health effect on children.”
The New Zealand Herald reported that in her Facebook post Hart-Murray wrote of the abuse of children from the time they were infants; middle-aged women born in New Zealand who needed interpreters because their parents were immigrants and they didn’t get an education; and a family of six who felt lucky their cousin was allowing them to stay in the single-car garage of the rundown state home he had just been given.
“Its old, cold, there’s no running water, there are rats and it’s mouldy,” Hart-Murray wrote of the garage. “The baby to come will sleep in the bed with the parents and three toddlers, unless I can find an alternative in time. At least the baby will be warm, but that’s not going to improve [the] atrocious rates of SUDI New Zealand has. It’s better than the relatives’ van in a dodgy carpark, where the parents take turns staying awake to protect [the children].”
Hart-Murray also said she would pay for important prescriptions herself from time to time because many families could not afford them once they had paid for food.
One pregnant teenager she saw was forced to live with a relative in a house where she had to share a bed with two teenage boys. Used needles and condoms were on the floor and there was a pile of used adult nappies and human excrement in the house, which didn’t have a toilet.
“I don’t think a lot of New Zealand is aware of what really goes on for so many people here in Aotearoa. It’s a largely hidden shame we’d rather not see.”
Hart-Murray is not working as a midwife after having had successful treatment for a benign tumour. She is now suffering cardiac trouble.
She said on her Facebook page that she had been overwhelmed by the response to the post from midwives who had the same stories to tell.
]]>Shocked award winner Jess Tiplady flew back to Auckland this morning clutching an enormous bouquet of flowers, a beautiful trophy and an enormous certificate.
The 29-year-old, who became a primary health NP in April, was awarded NZNO Young Nurse of the Year 2017 at the organisation’s annual conference dinner at Te Papa last night.
The young NP is one of only four NPs under 35 and Tiplady (whose mother is Ngāi Te Rangi) is currently the youngest Māori nurse to have achieved NP status in New Zealand.
To become an NP by age 29, Tiplady has studied every year but one since first enrolling in nursing school. “It’s been a massive journey to get to here,” acknowledges Tiplady. She said she was shocked by her win, was very grateful, and felt the award was a reflection of how much others have helped her on her journey.
Kerri Nuku, NZNO’s kaiwhakahaere, said when presenting the award to Tiplady that she was a great example of a nurse making a positive contribution to health outcomes for New Zealand children living in poverty. “The impact on families living in overcrowded houses, with the associated infection, itch and discomfort of eczema, loss of sleep and potential for hospitalisation, is significant,” said Nuku.
Tiplady has worked for Manurewa’s Greenstone Family Clinic since graduating in 2001 with a conjoint degree in nursing and health sciences from the University of Auckland.
Primary health has been her passion from the start and she says becoming an NP followed on from that passion as it seemed to be a “really useful tool”.
Early on at her time at Greenstone, she looked at how she could make a difference and saw a niche in helping prevent eczema crises for children and their families. “We were seeing a lot of children with nasty skin infections, and not sleeping and some very distressed children and parents.”
Around five years ago she started providing a nurse-led clinic in eczema for children to provide a whole package of care to support parents and reduce the risk of eczema flare-ups and distress.
A year later she set up an asthma clinic for children with the aim of using the clinical guidelines for good asthma care in primary health to see whether a focused clinic could make a difference to hospital admissions for asthma.
Invitations to the asthma clinic was tied in with the annual reminder letter sent to all children on preventative inhalers that it was time for their free flu vaccine. “We altered our annual letter to say come in and have a 30-minute appointment with a nurse to have your annual asthma check-up,” said Tiplady. “It was kind of a ‘warrant of fitness’ going into winter.”
She said in 2015 its practice admission rates for children with asthma halved compared with previous years, but it was very difficult to prove whether that was due to the asthma clinic or other factors. “But I think what we have managed to do is establish a really good model of care where our children are getting what is considered to be the best practice package of care for their asthma.”
Tiplady said about 80-110 children under 16 are eligible for the asthma clinic each year. She said she and other nurses chased up children where there might be barriers to coming into the clinic or grabbed an opportunistic clinic appointment if the child came into the practice for another reason.
While the young NP really likes working with children and young people – and has a special interest in mental health – her scope is primary care and her day-to-day work involves seeing a cross-section of patients across the practice’s population.
She also offers fortnightly clinics in James Cook High School and Alfriston College, predominantly in sexual health.
Tiplady was a member of the first cohort of the pilot Nurse Practitioner Training Programme (NPTP) and was mentored by two GPs at the Greenstone clinic. She said a particular aspect of NPTP that was particularly helpful was having two protected clinic days a week to focus on transitioning from being a nurse to being an NP.
After so many years of study, she says the focus for the next year was consolidating her knowledge and establishing herself in her role as an NP. “And then looking at where else I can utilise those skills as an NP. The clinical role is most important to me but the NP hat also offers the opportunity to do research, teaching and mentoring so I will look at where I can contribute in those areas.”
The Young Nurse of the Award was set up to recognise and celebrate the work of nurses in the younger age group and to encourage younger nurses to demonstrate their commitment to the nursing profession. The winner is chosen for showing compassion or courage beyond what is expected in their role as a nurse and who has improved care or health outcomes for their patients through their commitment to care, leadership, research or quality.
Kerri Nuku said she also warmly congratulated runner-up Dana Smith from Dunedin Hospital general surgery. Smith was nominated by her colleagues for her work in the community with children with Crohn’s disease including volunteering at their annual camps,” said.
The judging panel consisted of a representative from Otago University Centre for Postgraduate Nursing Studies, previous years’ award winners, the Ministry of Health’s Chief Nursing Officer (or representative), and the NZNO president and kaiwhakahaere.
]]>
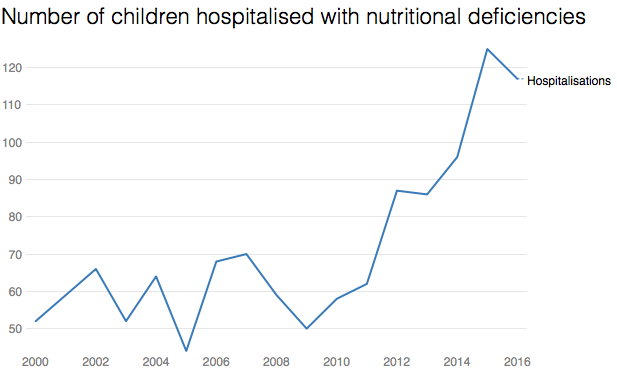
Child hospitalisation data shows around 120 children a year now have overnight stays due to nutritional deficiencies and anaemia, compared to an average 60 a decade ago.
Doctors say poor nutrition is also a factor in a significant proportion of the rest of the 40,000 annual child hospitalisations linked to poverty – and that vitamin deficiencies are more common in New Zealand compared to similar countries.
“Housing, stress and nutrition – it’s all tied together,” said pediatrician Dr Nikki Turner, from the Child Poverty Action Group. “If you want to eat nutritiously on a low-income it’s difficult, and that means you’re more likely to get sick and stay sick for longer.”
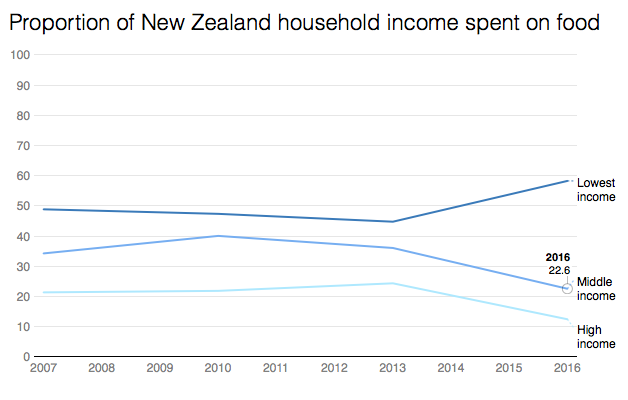
The new health data comes as food prices continue to rise, with the consumer price index last week indicating food costs were up 2.3 per cent on a year ago. At the same time, income in the poorest third of households has remained flat since 1982.
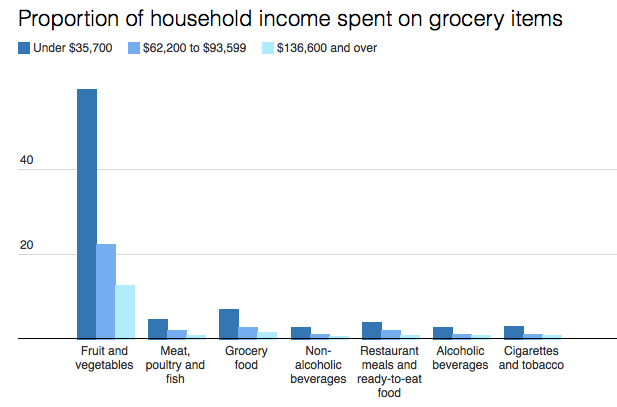
Statistics New Zealand information released to the Herald shows for families on the lowest incomes (under $35,000), that means they’re now spending 60 per cent of their income on food, compared to 48 per cent in 2007.
More than half of that goes on fruit and vegetables, data shows. Among middle-income families, 22 per cent of income goes on food, with one fifth of that on fruit and vegetables.
An Australian paper has suggested that “food stress” is believed to be experienced when more than 30 per cent of income is spent on groceries.
In practice, “food stress” means increasing reliance on food banks, charities, cheap “fillers” like white bread and noodles, or simply going without.
“I try to fill up the pantry but it only lasts one or two days and then it’s empty again,” said solo dad of three kids, Daniel*, from Otara. “I have to skip my own lunches because the kids are always hungry and I try to prioritise school lunches for them. I know that’s important.”
Dr Cameron Grant, the head of paediatrics at Auckland University, said it was rare for children to be hospitalised for severe nutritional issues in New Zealand, malnutrition was a factor in a significant proportion of illnesses.
“A third of children hospitalised at Starship have iron deficiency, for example,” Grant said. “A lack of vitamin D is also very common. That increases the risk of respiratory illnesses.”
New Zealand rates of iron deficiency are twice as high as Europe, the UK and Australia, he said, and Vitamin D deficiency was higher than the USA, because our food lacked nutrients.
However, New Zealand diets were also energy rich, meaning children could be both undernourished and obese – a situation that was not improving.
Child Poverty Action Group’s Turner said contrary to popular opinion, it wasn’t an issue of poor budgeting causing the problem.
According to household income data, low-income families spent about the same on cigarettes and alcohol as middle-income earners, for example.
“Low income families are not wasting money any more than anyone else, but it just doesn’t stretch far enough,” she said.
The University of Otago 2016 Food Survey estimates the basic weekly food cost for a man is $64 per week. For a woman it’s $55, and a 5-year-old is $40.
Research at the Auckland City Mission found families coming for food parcels have an average $24 per person each week for all groceries. That’s around $3.50 a day.
However, Massey University PhD candidate Rebekah Graham, who researches food insecurity, said some people had even less – such as one woman who had only $25 a week for herself and two children.
The food she bought – tinned fruit, bacon-and-egg pies, noodles – was barely enough to meet the family’s food requirements. Despite that, the woman still bought a cake as a gift for friend suffering a bereavement.
Graham’s research found families frequently had to make terrible choices to survive. One woman, surviving on $1 loaves of white bread, was unable to produce enough milk to feed her baby. Others put off urgent dental work. She also heard of people taking sleeping pills on a Friday so they could sleep through the weekend and not have to pay for food.
Chief executive of Variety, the Children’s Charity, Lorraine Taylor said food was always the first thing to go if families needed something – whether that was school uniforms or doctor’s bills. They also heard of parents not eating to feed their kids.
The charity, which runs a child sponsorship programme but is increasingly propping up families with food vouchers, said it was unacceptable that charities were left to fill the gap.
“Food should not be a negotiable. We want to live in a country where all Kiwi children are fed nutritious food.”
The Ministry of Health’s principal nutrition advisor Elizabeth Aitken said it last carried out a national children’s nutrition survey in 2002, and did not have more recent data on quantified nutrient intakes for children.
It said diet was just one of a range of causes of anaemia and nutritional deficiencies, but it knew obesity was increasing from poor quality diets.
The ministry had a range of programmes to help parents with advice on nutrition and development, she said.
Daniel’s family
The kids are always hungry at Daniel’s house, but the cupboards are almost never full.
A solo dad to three school-aged kids, he struggles to make the groceries last the week, even though he skips his own lunches and uses all the leftovers – and attended a budgeting course to learn how to make money go further.
“Sometimes I have to lock the cupboard to make sure we have enough,” he says. “I find it hard.”
Daniel – which is not his real name – has at most $200 to spend a week on food, depending on bills or how much work he gets. He earns about $500 a week. His rent it $180, for a three-bedroom in Otara.
The only fruit he buys are apples and oranges, even though his kids love grapes, and they eat toast and spaghetti for dinner most nights a week. A cooked chicken is a luxury, only for special occasions. The kids never buy their lunches, instead having bread and cheese, maybe a muesli bar, and a piece of fruit.
“I know it doesn’t look good if they don’t have lunch,” Daniel says. “I have to skip my own lunches because the kids are always hungry and I try to prioritise school lunches for them. I know that’s important.”
A sponsorship – through the charity Variety – has helped, helping with the children’s shoes and clothes, and occasional supermarket vouchers.
Sometimes, however, the bills push him to line up at the food bank for a parcel, even thought he hates it.
“I feel embarrassed at times, but I just had to tell myself that we are desperate,” he says. “I have no choice.”
]]>