“Embarrassment, shyness about being examined and talking about “private” bodily functions or simply not knowing the signs of bowel cancer until it is too late is a major problem in New Zealand. I want to change that, so we can help save lives by encouraging people to get help early,” she said.
New Zealand has one of the highest incidences of bowel cancer in the world. Each year about 3,000 people are diagnosed with the disease and more than 1,200 will die. Bowel cancer is the second highest cause of cancer death in New Zealand, but it can be treated successfully if it is detected and treated early.
“We have evidence that shows that nearly 30 percent of patients with bowel cancer, including a high proportion of Maori and Pacific Island people, turn up at an emergency department or at their GP’s surgery displaying acute symptoms which they have not associated with cancer,” Warren said.
“They think they just have a really sore tummy, bleeding piles (haemorrhoids) or pulled a muscle and done nothing about it until they are very unwell when bowel cancer, if diagnosed and treated early, has a high rate of favourable outcomes.”
Warren, is the recent recipient of the Cancer Research Trust New Zealand Clinical Fellowship for Nurses, and is working on her PhD exploring why some people delay seeking help once symptoms occur and to identify new approaches to promote awareness of signs of the disease and encourage earlier help.
“This study will be the first of its kind to map routes to diagnosis for colorectal cancer in New Zealand,” she said. “It will provide insight to areas for person and system level interventions that can be tested in future studies to minimise emergency department and late presentations of colorectal cancer in New Zealand.”
The study will follow two groups of patients diagnosed with colorectal cancer at a rural hospital in the Wairarapa and Wellington’s Capital and Coast Hospital and look at a myriad of influences that can act as a deterrent to seeking the right help at the right time. These include low literacy and health awareness, cultural, socio-demographic factors, attitudes and personal inhibitions and fears.
In funding the study, the Cancer Research Trust recognised the importance of the work as low public awareness of bowel cancer signs and symptoms can result in delays in diagnosis and starting treatment – sometimes with devastating consequences. The Cancer Research Trust, a registered charity, uses every dollar donated to fund New Zealand-based initiatives for improvements in prevention, detection, diagnosis or treatment of all types of cancer, or in palliative care.
Source: Cancer Research Trust New Zealand
FURTHER INFORMATION
What is Bowel Cancer?
Bowel cancer is a malignant growth that develops inside the bowel. It is also called colon, rectal or colorectal cancer
What are the Symptoms?
- Bleeding from the bottom (rectal bleeding) without any obvious reason, or other symptoms such as straining, soreness, lumps
- A persistent change in bowel habit for several weeks – going to the toilet more often or experiencing looser stools, diarrhoea or constipation
- Abdominal pain especially if severe
- Any lumps or mass in your tummy
- Weight loss and feeling weak and tired (a symptom of anaemia)
How do I help myself?
- Be aware of the symptoms.
- If in doubt seek help – remember bowel cancer is curable if treated early.
- Don’t be shy or embarrassed
- Go to the doctor immediately
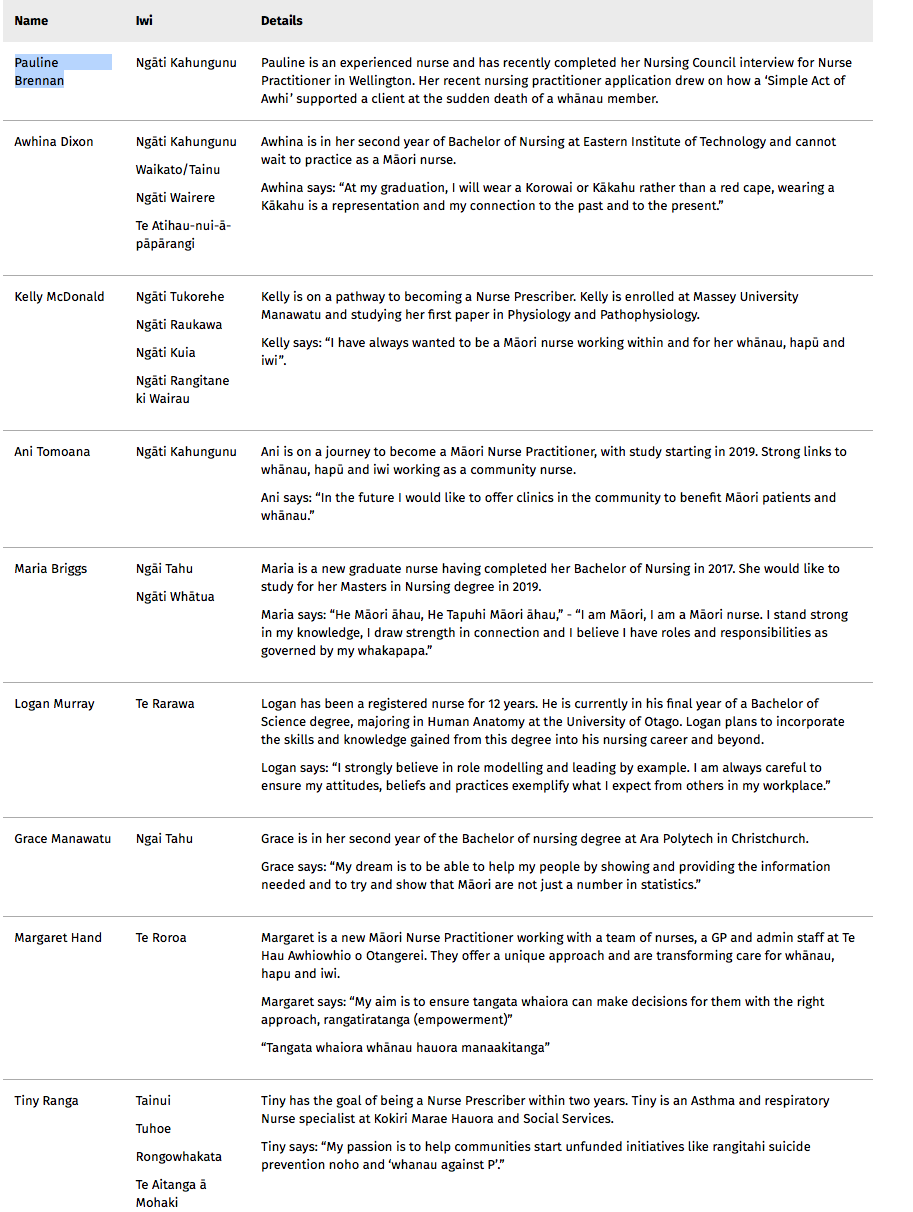
The Tapuhi Kaitiaki Awards recognise Māori nurses who are furthering their studies, clinical practice and professional development while continuing to support the wellbeing of whānau, hapū and iwi.
“Māori nurses play a unique role in the health sector in that they are both clinically and culturally competent health professionals,” said NZNO Kaiwhakahaere Kerri Nuku on the new awards.
Alison Hill, Pharmac’s Director of Engagement and Implementation said a Pharmac goal was eliminate inequities in access to medicines by 2025, and improving Māori health outcomes was a key focus.
“Māori health professionals have a pivotal role in helping Māori understand and access the medicines they need,” said Hill.
“We were really pleased with the quality of the applications, which painted a vivid picture of the deep understanding and strong commitment these nurses have to serving their communities through their profession. I was impressed to see how much these nurses fit into their daily lives, juggling their studies, tamariki, home and professional lives.
She said each of the nine winners demonstrated strong connections and dedication to their whakapapa and community, while continuing to strive towards excellence in their studies or professional practice.
Recipients of the 2018 Tapuhi Kaitiaki awards each received $2000 to $2500.
Nominations for the first Tapuhi Kaitiaki Awards will close on July 10 and announced at the Indigenous Nurses Conference in Auckland on 11 August 2018.
Pharmac and Te Pōari o Te Rūnanga o Aotearoa of the New Zealand Nurse Organisation launched the awards recently with Pharmac chief executive Sarah Fitt saying the awards acknowledged the role that Māori nurses have as key influencers and role models.
“For whānau, the Māori nurse with the knowledge, expertise and understanding of tikanga, kawa, Māori health needs and practise is an important advocate and support person,” said Fitt. “These awards are a financial contribution for all Māori nurses to further their studies and clinical practise, and can be used by nurses to help support their work load and whānau commitments.”
Kerri Nuku, NZNO’s Kaiwhakahaere, said the awards were a great opportunity to acknowledge Māori nurses’ uniqueness.
“Undertaking further academic study and training to become nurse prescribers and nurse practitioners is a huge commitment on top of everyday mahi and whānau life,” said Nuku.
“Te Rūnanga are extremely proud of the support and investment PHARMAC is providing with the Tapuhi Kaitiaki scholarships and we believe this will help whānau, hapū and iwi to access and understand their medicines.”
“Māori nurses are great innovators, it’s a great opportunity to showcase ways in which they work day-to-day for the betterment of their people, hei oranga motuhake mo ngā whānau, me ngā hapū, me ngā iwi.”
The scholarships will be awarded in two categories:
- Nurse prescriber/nurse practitioner – to support nurses on the journey to become RN prescribers or NPs by offering financial support for their study and clinical practice requirements
- Māori nurse Mātauranga Award–to support nurses wanting to further their study and/or would like to develop an innovative way to assist whānau, hapū and iwi to access and understand their medicines. It is also available to enrolled nurses who wish to study toward registered nurse status.
Application forms and more information can be found here
]]>From July 2018 the initiative will see Victoria’s Dr Robyn Maude and Dr Ausaga Faasalele Tanuvasa from the University’s Faculty of Health, deliver five PhDs, eight Master’s degrees and up to 40 diploma and certificate courses in Sāmoa. Implementation of the programme at NUS is being led by the Vice-Chancellor Professor Fui Le’apai Tu’ua ‘Ilaoa Asofou So’o and Dean of the Faculty of Health Sciences Soi Salā Ma’atasesa Samuelu-Matthes.
Victoria’s Associate Professor Hon Luamanuvao Winnie Laban, Assistant Vice-Chancellor (Pasifika), says the ability to continue their studies in Sāmoa will enable students to remain working in the community, support their families and actively contributing to policy, practice and teaching. “We want to help enhance the resilience of the Sāmoan people through best practice and primary health care – fa’a Sāmoa, so it is essential that research is undertaken by Sāmoans in Sāmoa on Sāmoan issues,” she says.
“The ultimate objective is the provision of appropriate postgraduate qualifications by NUS to ensure nurses, midwives and other health professionals have equality of access to study, which will allow them to identify research issues and develop solutions relevant to Sāmoa in a manner that best allows them to serve the Sāmoan people.”
Gary Ward, Manager of Knowledge Transfer Services at Viclink, Victoria University’s commercialisation arm, worked closely with Victoria’s Dr Kathy Holloway to support the University’s Graduate School of Nursing, Midwifery and Health through the establishment process. “We worked with NUS to define clear success criteria. If a model or option didn’t meet our partners’ and stakeholders’ needs it was discarded. As a result Growing our Own has the full support and belief of all stakeholders across the education and health sectors in Sāmoa,” he says.
The Prime Minister of Sāmoa, the Hon. Tuilaepa Fatialofa Lupesoliai Dr Sailele Malielegaoi, has been a fundamental supporter of the programme due to its alignment with his vision for improved primary health care. He said 2018 was a poignant time to launch the programme as Sāmoa was both remembering 100 years since the influenza pandemic decimated 22 percent of its population and celebrating 100 years since the nursing profession was established in Sāmoa.
Holloway said it was an exciting opportunity to work with our Sāmoan colleagues to grow their own nurses and midwives, to stay at home and strengthen their own health system and to serve their people fa’a Sāmoa.”
]]>
The appointment of new members – Maria Armstrong and Joanna Hart – has just been confirmed by the Minister of Health after the results of last year’s Nursing Council election were delayed by the change of Government. The Minister has also re-appointed current chair Catherine Byrne to the Council.
The two new members were amongst 16 nurses who put themselves forward for the three elected health practitioner positions on the nine member council – including sitting council members Catherine Byrne, Jo Ann Walton (who was deputy chair at the time) and Joanne Hopson. Walton later withdrew from the election process and from her place on the council as she is now a council employee having taken up the post of Director, Registrant Quality.
Joanna (Jo) Hart, a Bay of Plenty registered nurse with 20 years’ experience, stood for the Council on the platform of the Council not only protecting the public but also protecting nurses from the “overwhelming expectations” for further study. “I’ve seen my colleagues despair at overwhelming expectations to further their education, along with annual increases in PDRP (professional development and recognition programme) requirements and I’ve experienced them too,” she wrote in her election candidate’s bio.
The second new Council member is Maria Armstrong, who is a charge nurse at the Auckland District Health Board and a director on the board of the New Zealand Nurses Organisation.
Armstrong, who has a clinical masters degree in nursing, also talked in her candidate bio about balancing the public good with the challenges facing nursing as a profession from changing practice roles and expectations in a changing healthcare environment.
“These changes are increasing both the professional and the personal demands of nurses,” said Armstrong in her bio. “I have a good understanding of the challenges we face moving forward and will promote measures to facilitate achievement of the inter-linked objectives of optimal nursing care for the public good and the lived experience of nursing for members of the profession.”
The Nursing Council in a statement said they sincerely thanked the outgoing members of Council for their dedicated service to the Council and the nursing profession. The council has appointed To’a Fereti as the new deputy chair.
Just over 10 per cent of eligible nurses voted in the 2017 election – the same turnout as the elections held in 2011 and 2014. The online Council election closed on September 1 and were then caught up with the government elections and change of government as the Nursing Council was unable to announce the elected council members until the Minister of Health had approved the nominated candidates and the nominations had gone through the government’s Appointments Committee.
]]>It is certainly heartening to see that there were very high completion rates and high pass rates. It is a tough course and anyone who has done the prescribing papers will tell you that.
I think the report has pretty much hit the nail on the head. The tying of entry onto the course with a job at the end, has no doubt inspired those on the course and got employers to think about the business case before the person graduates.
I completed the pathway far faster than my DHB thought and I had to wait 13 months between becoming an NP and starting in the role.
It should also be noted that the NPTP had students from across New Zealand – from Dunedin to Kaitaia, and that about 50% of all students were from primary care settings, which mirrors the distribution of NPs in the work place. The funding following the student (rather than the usual bulk funding to DHBs for prescribing practicums) promoted more primary care NP Interns and those from rural areas, which is where the demand will be.
One thing that needs to be considered is the evaluation report noting the disparity between employers noting changes in confidence and competence in the NPTP graduates despite the graduates own self-assessment being tougher on themselves.
For me, as Chair of NPNZ, I am always struck by the humility of NPs and by their awareness of the enormity of the responsibility on their shoulders, so that finding did not surprise me. NPs are good at knowing where their boundaries are and knowing what they don’t know.
Do you think the NPTP scheme should expand both in numbers and providers i.e. beyond the current two providers (The University of Auckland and Massey University) and 20 funded places.
We are a long way short of the numbers of NPs estimated to be needed to cover the delivery of healthcare.
For example Nelson/Marlborough District Health Board has gone from ‘half’ an NP (0.5 fulltime equivalent) to nine NP FTE in two years, and still needs to grow more to meet the needs of the community.
We also have to factor in that we are 17 years in from registering the first NP so now those experienced RN’s who became NPs will be starting to retire, and the issue of succession planning needs to be considered.
I would be keen to know if the subsequent courses were over-subscribed. The aged care and primary health sectors will continue to grow and place heavy demand on health services.
We are still in the situation of that if you want an NP then you must grow your own. I am not sure we will ever get to the point of over-producing NPs – even if we add an extra 10-20 NPTP places. Alongside the NPTP cohort are students on the usual Health Workforce New Zealand (HWNZ) pathway but they don’t have to have an employer agreement for a job at the end of their clinical masters’ degree.
In terms of providers I did my clinical papers in Christchurch so think it would be good to see a South Island provider. We are a very rural and remote populace on the whole and there are opportunities for NPs out there.
What did you think of the evaluation’s comment that an ongoing barrier to the NP workforce is “lack of awareness, understanding and acceptance of the NP role”?
It always takes a new role time to bed in.
We are looking at a health system that has been around for a while and the role boundaries have been very fixed for a long time; so the media, the general population and even the health system will be challenged in how to best manage, support and utilise this new resource.
Within Southern DHB (where I am based) we have a development group, this initially was for NP role development and has now expanded to look at the opportunities for RN prescribing.
Workforce development and funding has been a little too much based on historic service delivery and also on the personalities, personal preferences and effectiveness of those in the senior nursing roles. I would like to see a more analytic approach to that.
The Ministry of Health are doing great work, their release of the factsheet, Nurse Practitioners In New Zealand in October 2017 helped clarify what we do.
The work of the Nursing Council on the NP competencies and broadening the scope can also not be under-rated. That work, along with the work on registered nurse (RN) prescribing, has opened clear paths for those nurses who want either a narrow, often disease-specific focus, or those who want a broader focus with the authorised prescribing responsibilities of the Nurse Practitioner.
The work Nursing Council did on streamlining portfolios was of immense benefit for those coming through, it was seen by many as one hurdle too many and often the size of the task was over-estimated as there wasn’t much guidance.
The Nurse Practitioners New Zealand (NPNZ) group are constantly working on those issues and barriers. Often with those institutions outside of health they do not know what NPs are or what we do. When we talk to them they usually get it and the barrier – to our practice and also to the patient getting an equitable service – disappears.
Within the last year we have seen national meetings held for the mental mealth NPs, the emergency department NPs and soon the haematology/oncology NPs are having their first national meeting too. We have also been working on getting the regional NP support groups going (this remains a work in progress) in order that support and mentoring is available not only for NP graduates but also those on the pathway.
Another issue raised in the report of interest was that providing clinical supervision for GP registrars’ pays more and – when we look at the disparity in HWNZ funding between medicine and the other health professions – it is not hard to see why that is.
This is the same issue with continuing education for nurse practitioners there are no real postgraduate courses aimed at qualified NPs.
NPNZ has been having discussions with organisations that provide medical postgraduate education around accessing resources, as NPs need to know pretty much the same things. Those discussions have been very productive, but like any paradigm shift it takes time.
It was disappointing, but not unexpected, that the recent New Zealand Nurses Organisation/DHBs MECA negotiations didn’t make progress on continuing education money. Because the NPTP evaluation report accurately stated there is a disparity between access to continuing education between DHB and non-DHB employees, between DHBs, and also between NPs and our medical colleagues.
NPs are expected by Nursing Council to keep up to date, but with no resources and no funding this is difficult.
Another avenue through which this issue can be addressed is via the Health Practitioners Competence Assurance Amendment Bill, as Clause 27 of the bill currently before parliament “requires an authority to promote and facilitate interdisciplinary collaboration and co-operation in the delivery of Health services..” This would include the Nursing Council and Medical Council, amongst others, promoting interdisciplinary collaboration.
Any other comments on the report or the Ministry of Health’s request for feedback on how to develop the role of NPs?
In terms of the mentoring, the College of Nurses have produced some great resources. Also as we have just short 300 nurse practitioners with a current annual practising certificate (APC) we will have more NPs available for mentoring nurses on the NP pathway.
The issue of back-filling is an interesting one, not only do people struggle while on the NP pathway, but also once they are an NP.
In primary care NPs, on the whole, are employed to help make money for the business, so time off for peer groups, supervision or training is an issue. Again that would require funding to deal with that issue.
This is also an issue in secondary care- there aren’t the NPs to take over from you if you want a sabbatical or are sick.
This may improve as the numbers build.
One colleague stated that there was also no evidence of the mentioned honorarium for NPTP clinical supervisors being paid? There is also a time impact on the clinical supervisors involved in training NPs which I wonder whether is fully acknowledged?
]]>
The scholarships provide financial assistance – $10,000 for medical and dentistry students and $5000 for other health-related courses – to Pacific students who are committed to improving Pacific health. Applications are considered from both full-time and part-time workers (including district health board employees).
More information on the criteria and the online application form can be found here.
Applications close on February 6 2018.
]]>More than 130 rural nurses took part in the online survey held earlier this year by the newly formed Rural Nurses NZ working party.
Rhonda Johnson, chair of the Rural Nurses NZ working party, said the survey findings confirmed some of her hunches and provided a platform to help develop an action plan for the group that came into being after March’s National Rural Health Conference. She said the group also remained keen to get a better grasp of the total number of rural nurses and was looking to do its own census by directly contacting rural hospitals, practices and health providers
The group’s online survey found that 79 per cent of respondents had completed some form of postgraduate education and 21 per cent had a master’s degree or were nurse practitioners. About 91 per cent of respondents accessed professional development online and nearly 60 per cent faced non-physical barriers to accessing professional development including funding, travel and accommodation costs and lack of cover or time to attend.
“We’ve listened to rural nurses and what it is they need and they want – and professional development is one of those issues,” said Johnson. “Obviously location is a big part of accessing professional development, and we hope to establish links, networks and connections with each other so we support each with professional development as well.
“I was probably pleasantly surprised by the numbers who have completed some kind of postgraduate education – I thought that was a real bonus for rural nursing and shows the calibre.” She said it might also reflect a trend across the whole profession, with postgraduate education being seen as important for maintaining competency.
“Obviously it is an ageing workforce, but again that is true of nursing as a whole.” What she hadn’t expected was that – despite the largest group of respondents being in the 55-64-year-old age bracket (38 per cent) and 56 per cent having been registered for more than 25 years – that the largest group of respondents had only been practising rurally for up to five years (27 per cent) and only four per cent had worked rurally for more than 20 years.
“When I actually thought about my own working environment [Central Otago’s Dunstan Hospital], although there is a stable workforce of mature nurses there are also a number of younger nurses coming through.”
She said to her the survey findings confirmed the need for a group like theirs to be in existence to advocate for rural nurses, provide mentorship and connection between rural nurses working in other contexts and places, and influence other nurses to think about rural nursing as a career path. “We want to help influence recruitment and retention in these areas which are often hard to staff.”
The survey also indicated that the vast majority of respondents faced various difficulties in transporting patients to a base hospital due to inclement weather and lack of transport, and some required a boat or plane to transport patients.
Johnson said a list of working items had been collated following the survey findings and members suggestions and would be prioritised for action.
She said the RNNZ group was also working on a mission statement and how the group will fit with existing rural groups. “We don’t want to reinvent the wheel; connections with other rural groups, like the Rural Hospital Network (RHN) and Rural General Practice Network (RGPN), are important and we are working on those at the moment.” (See RNNZ’s term of references’ purposes and objectives below.)
As part of that work, the group remains keen to get a clearer picture of the number of nurses working rurally. Johnson said the Nursing Council does provide a setting category of ‘rural’ when gathering data during annual practising certificate renewals, but most rural nurses tick settings like ‘practice nursing’ or ‘hospital’.
“So the Nursing Council data shows only 257 rural nurses working in New Zealand, but that is grossly under-represented so we need to find out how many rural nurses there are. Which may sound quite easy, but actually it is not – because the term ‘rural’ is not adequately defined.”
Johnson said there is a research proposal on the table by rural hospital doctor Garry Nixon to define the term ‘rural’, which would help with establishing a rural health workforce database.
But in the interim, the working party was looking to do its own work to get a ‘ball park’ figure by contacting hospitals, general practices and other health providers in a rural setting to find out how many nurses they employ. She said at present the Rural Nurses NZ membership is open to any nurse who believes they practise in a rural context.
Currently the working party, which includes nurses from the Far North to Stewart Island (see bios below), meet via a monthly video conference. Johnson said the aim was for all working party committee members to attend the next Rural Health Conference in Auckland in March.
RURAL NURSES NEW ZEALAND (RNNZ)
Purpose
To provide a regular forum that enables a diverse group of rural nurses from across New Zealand to develop models and/or strategies to support rural and remote nurses, including:
- Establish and maintain networking opportunities.
- Positively influence retention and recruitment of nurses in rural areas, including new graduate support.
- Contribute to the standardisation of standing orders for rural New Zealand.
- Collaboration with other organisations.
- Influence a recognised career pathway for rural nurses.
- Support development of rural nurse supervision.
- Build knowledge of the needs of rural nurses in New Zealand.
Objectives
- To advocate for, with, and on behalf of rural nurses in New Zealand.
- To support a means of providing consistent clinical direction and support to rural nurses particularly those working in isolation.
- To enhance networking of rural nurses within already established forums.
- To create innovative ways of bringing rural nurses together.
Rural nurses work in a broad variety of environments, including, but not limited to: general practice, hospital, public heath, occupational health, district, PRIME, residential care, palliative care, nurse specialist or nurse practitioner roles, mental health, LMC, Plunket, wellchild, whānau ora, long-term conditions, and nurse-led clinics.
RNNZ MEMBER BIOGRAPHIES
Rhonda Johnson: Chairperson
I have been immersed in rural nursing since 2002 and held the role of charge nurse at Dunstan Hospital for a total of 11 years. I recently moved into project planning and am now involved in the early stages of the Dunedin Hospital redevelopment project. I bring my rural knowledge and experience to this role.
I love the diversity and challenge that rurality brings and am committed to supporting staff and guiding professional practice in our unique context. I completed my PG Dip through the Rural Institute of Health and University of Auckland in 2008 and am now working toward my Masters of Nursing. I see the benefits of increasing the rural nurse profile in New Zealand and a need to establish better connections across the country to develop initiatives key to rural nurses in all contexts. I am currently on the Rural Hospital Network (RHN) executive team and am enjoying the new challenge of working with our enthusiastic group of rural nurses on the working party.
Emma Dillon: Secretary
Up until this winter I was working in Colville, a small village 30 minutes north of Coromandel, for two years. With an enrolled population of 700 patients, the clinic is owned/operated by a sole GP and employs two nurses plus support staff. Working as a rural nurse here includes practice nursing, district nursing, public health, palliative care and after hours/PRIME nursing. I was born and raised on the south coast of the South Island, and graduated with a nursing degree from CPIT in Christchurch in 2010.
Currently I am studying at the University of Otago, Christchurch, doing my PG Dip specialising in rural nursing. In late August I moved back to the deep south to take on the exciting challenge of working as a rural nurse specialist based mostly on Stewart Island, and in Tokanui in the Catlins.
Kate Stark: Communication Liason
Currently I work as a nurse practitioner (NP) at Gore Health Centre, part of an IHCF in rural Eastern Southland. I also work as an NP/PRIME Practitioner in Twizel, South Canterbury, and Central Otago. Prior to this, I worked in Roxburgh and Tapanui in rural primary healthcare. I am currently on the RGPN executive committee and hold the following positions of external nursing representative on behalf of the CPHCN:
- Liaison Rural GP Network (RGPN)
- Member Rural Health Advisory Group (NZRHAG)
- National PRIME Review Steering Group
- PRIME Clinical Governance Working Party
- NASO Air Ambulance Co-Design Clinical Advisory Group
I believe it is crucial to improve the heathcare of rural populations and to reduce the barriers for the health of rural people while simultaneously working for rural nurses to promote the unique role that rural nurses carry out individually and in teams. I am delighted to be involved in RNNZ and look forward to making a difference to rural nurses working in all contexts.
Virginia Maskill
Since graduating as an RComp.N in 1992, I have worked in a variety of clinical settings including the Nelson-Marlborough District Health Board. During this time I gained significant experience working in rural settings, including a dual role as an ambulance officer/registered nurse in a busy accident and emergency department and after-hours general practitioner service. For six of these years I was also employed part-time at the hospital’s alcohol and drug outpatient clinic as a registered nurse/counsellor. These positions provided me with extensive experience of the challenges specific to rural nursing due to wide geographical regions and a dispersed population often under-serviced with health resources.
In 2009 I joined the Centre for Postgraduate Nursing Studies at the University of Otago, Christchurch and the Department of Psychological Medicine, University of Otago, Christchurch from 2006 to 2016. I have a special research interest in the rural nursing workforce, hence my keenness to contribute to the Rural Nurses New Zealand working party. I am currently a member of the Rural Health Plan Working Group for the future development of rural health, Division of Health Sciences, University of Otago.
Cathy Beazley
Tena koutou katoa. Ko Cathy Beazley toku ingoa.
I began working as a nurse practitioner in 2013 and currently work in primary health care for Hokianga Health (a Māori provider) in the remote north-west of the North Island. Hokianga Health provides health care for an enrolled population of about 6,350, plus the all-year-round visitors.
Having started work in rural practice in 2000, I have gained experience in a number of positions, including working as an inpatient RN on small acute ward, rural practice nursing and community nursing.
At a local level I am a member of our rural GP, Clinical Governance and Significant Event groups. Regionally I am a member of the Primary Options Programme Northland group and Manaaki Manawa Heart Care Clinical Governance Group. I am also involved in a new rural research project, focused on the impact of introducing a haematology analyser at a rural hospital. I believe we need to work collectively to inspire future growth of this particular area of specialist nursing and I look forward to being part of Rural Nurses New Zealand.
Rhoena Davis
I am a nurse practitioner working in the northern rural area of Whangaroa in Whānau Ora. I have been an NP for eight years, working in rural areas for approximately 25 years.
I have completed a Master in Clinical Advanced Nursing with First Class Honours through Auckland University and my Expert PDRP for Primary Health Care. I have completed a Postgraduate Diploma in Māori Business Studies through Auckland University, Postgraduate Certificate in Well Child Health through Whitireia Polytechnic, Graduate Certificate in Specialty Nursing Practice (Child and Family Health) and a Graduate Certificate in Nursing Practice (Public Health).
I am excited about what the newly formed Rural Nurses New Zealand working party can offer rural nurses and am already enjoying being involved.
Debi Lawry
I came to rural nursing late in my career after spending much of my nursing life working in Auckland. I have been a bedside (incubator side) nurse, a clinical nurse educator, a charge nurse and a nurse consultant. Along the way I also became a midwife. I completed an Advanced Diploma in Nursing and have since had a varied academic journey with a number of post graduate papers in neonatal science, health management, ethics and health policy. I moved to Dunedin in 2002 to help establish the newly created nurse director role. Five years later I achieved my dream of moving to Central Otago and working at Dunstan Hospital.
My eyes were opened to the complexities, challenges and joys of rural healthcare. Much of my career has been spent in nursing leadership roles where I strive to ensure nurses have the education, resources (human and consumables), skills and equipment to do their job well.
I am now very keen to be part of a working party to identify the issues for rural nurses, particularly hospital nurses (but not exclusively so) and to advance our cause.
Christine Dorsey
Kia ora. Ko Christine Dorsey toku ingoa.
I live in the Hokianga, in rural North Island. I am currently employed at Hokianga Health as the Hospital Services Manager for our small rural hospital. My roles include overseeing the 24/7 accident and emergency, acute inpatients, and residential care services.
My background is in emergency care and midwifery across both primary and secondary care.
At an organisational level I am a member of the executive team and co-ordinate internal meetings and ongoing professional development for staff. I am also currently the chairperson for the South Hokianga St John – an endangered service in the current climate.
With regards to rural nursing, my interests are in developing standardised clinical guidelines and standing orders for safe, effective use in rural New Zealand. In addition to this, I am supportive of further work and resources to improve easily accessible professional development options for rural nurses, something that is one of the aims for the Rural Nurses New Zealand group, hence I am very pleased to be involved.
Rachael Pretorius
My name is Rachael Pretorius and I am a nurse practitioner working in a rural general practice in Martinborough, South Wairarapa, where I have worked for the last two years. I am also PRIME trained. I am acutely aware of the issues that impact on rural living, nursing, and practice. Living and working in a rural area means working to the top of your scope, dealing with everything that comes through the doors, hoping your internet will work at home (or work) and that you might be able to do some online learning sometime, and hoping the roads aren’t flooded out so patients can get to the practice over gravel roads.
I am the College of Nurses representative for the Rural Health Alliance Aotearoa New Zealand (RHAANZ) and a RHAANZ council member.
I love working in a rural practice. Even though I haven’t lived in rural New Zealand for very long, I know what we miss out on compared with our city counterparts and I think a rural nurse working party is an excellent way for rural nurses to get their voices heard and ensure that rural nurses enjoy the same support that urban nurses do.
]]>
Doctoral researcher Jennifer Roberts is asking for nurse educators to take part in an anonymous survey about their preparedness and experiences of working with Māori nursing students in nursing schools.
Roberts is head of EIT’s School of Nursing, which has a high percentage of its nursing student population identifying as Māori – about a third in its Hawke’s Bay campus and about half in Gisborne.
“It’s an important study body for us in our region and we take that responsibility seriously given the national emphasis on growing the Māori nursing workforce.”
In 2015 the HWNZ Nursing Workforce Governance Group set a date of 2028 for the Māori nursing workforce to match the percentage of Māori in the population with the goal of helping improve access to quality health care for Māori. (Currently nurses identifying as Māori make up about six per cent of the nursing workforce, while Māori are 15 per cent of the New Zealand population.)
Roberts said she initially considered looking at what were the barriers and enablers for Māori nursing students’ success for her doctoral research topic. A literature search discovered that a lot of work had been done in that area but where there was a gap in knowledge was how nurses educators and nursing schools worked with Māori nursing students.
So she decided to flip the question around and focus on how nursing education practice in nursing schools and institutes may be contributing or inhibiting Māori student success. “And success is more than just achieving the qualification, it is about having a positive experience through learning as well,” said Roberts.
She said little was known about nursing educators’ preparedness for working with Māori students or their experiences in doing so.
“As (nursing) lecturers I think we all understand the importance of cultural safety in nursing practice,” said Roberts. But she wondered how that translated into how teachers themselves taught and interacted with student nurses. “Are we (ourselves) culturally safe in the classroom?”.
Roberts said if you look at the population of nurse educators, most were Pakeha like herself. “I think so many of us are well intentioned, but we maybe don’t have the tools…” said Roberts. “We want to do a good job, but are we?” She stressed it was “not a witch-hunt in any way” and instead her research’s aim was to help figure out how best to equip the nurse educator workforce to deal with cultural aspects of education.
Roberts said helpful work had been done by Ngā Manukura o Āpōpō – a workforce project to foster the professional development of Māori nurses and midwives that has included publishing performance scorecards of nursing schools. Informal work had also been done by NETS (Nursing Education in the Tertiary Sector) looking at what systems nursing schools had in place for supporting Māori students. Roberts’ work was to focus on the preparation and experience of nurse educators
She is inviting nurses currently working in undergraduate nursing education as nursing lecturers, nursing programme co-ordinators or undergraduate nursing programme managers to take part in an online survey and/or interviews.
Her research questions include:
- What are the institutional and school strategies that seek to support Māori nursing students?
- What are nurse leaders’ and educators’ perceptions of barriers and enablers in providing nursing education to Māori nursing students?
- How do nurse educators understand and interpret cultural safety in nursing education?
- How do nurse educators practice and apply the concepts of cultural safety in nursing education?
Nurse educators who wish to take part in the anonymous questionnaire can click here or email Jennifer Roberts to find out more.
]]>
Sue Hayward, director of nursing at Waikato DHB, said the DHB was presented with the award at the recent Health Roundtable Nursing Improvement meeting in recognition of achievement in the area of “sustainable and sustained leadership development and career progression”.
Waikato’s leadership development includes a programme launched in 2013 of shoulder-tapping new nurses with leadership potential to join a leadership programme run in league with the University of Auckland that involves mentoring, postgraduate study and practice-based research projects.
Hayward said its overall nursing leadership framework was underpinned by local and regional DHB leadership programmes and also included access to postgraduate learning as there was a “fundamental expectation that each individual nurse – regardless of expertise level or designated role – must lead where they stand”.
“The involvement and active participation in ward-based quality improvement activities, peer support, preceptering and delivering learnings from an event are all seen as leadership and recognised as such,” said Hayward. “Confidence builds and of course that can be a great springboard into other nursing roles.”
]]>