The Ministry of Health announced this week that Broodkoorn, of Ngāpuhi and Dutch whakapapa, had been appointed to the role. She is believed to be the first chief nurse of Māori descent since the forerunner of the role was created nearly a century ago. Her appointment follows the resignation of Dr Jane O’Malley, who left the Ministry in February to take up the role of Plunket’s first chief nurse.
Broodkoorn, who has been director of nursing and midwifery at Northland DHB since 2010, told Nursing Reviewsaid she was feeling very excited – and a little nervous – about the opportunities and potential of the senior national role, but also sad at leaving Northland.
“It is an honour to represent nursing and be the first Māori nurse to be appointed to a role like this,” said Broodkoorn. She said she had also been humbled by the amount of texts, emails, phonecalls, tweets and Facebook messages from colleagues, friends and family from across New Zealand but also overseas.
New-look Ministry
In February she will join the country’s first Chief Allied Health Professions Officer Martin Chadwick and Chief Medical Officer Dr Andrew Simpson in the new ‘Clinical Cluster’ created as part of a restructuring of the ministry management team, carried out by new Director General of Health Dr Ashley Bloomfield, that came into effect in October.
Broodkoorn, is excited to be joining the Ministry under Bloomfield’s leadership and said she shared his commitment to achieving health equity in outcomes across the country which would also be one of her big priorities in her new role.
“I believe nursing is well placed to contribute to that – I think we need to ensure that nursing is leading that change and in order to do that we need a sustainable nursing workforce that is future focused and prepared for that change.”
She said to do that nursing needed a robust workforce pipeline from ensuring future nurses have the right school preparation through to supporting new graduate nurses once trained and retaining them in the workforce. Also on her agenda was how to further develop more advanced and expanded nursing roles in the three scopes of practice – registered nurses, enrolled nurses and nurse practitioners. “And of course on the radar is (doing the same) for our Māori and Pacific nursing workforce.”
“Also how do we add value as a profession where we work as a team and work with our other professional colleagues and clinical partners to contribute the leadership of the health and social sector as a whole.”
Wearing two hats
Broodkoorn said she applied for the role for a number of reasons – including being encouraged by a number of people – and the chance to represent nursing as a Māori nurse. She has been clinical lead for Ngā Manukura o Āpōpō – the national Māori nursing and midwifery workforce development programme.
“It is my passion to encourage others to be able to be ready and step up into roles like this. And if I wasn’t prepared to do that myself I shouldn’t be asking that of others.” Also she recognised the importance of having a New Zealand and a Māori nurse in the role.
“I think Māori nursing has been asking for it for some time – in terms of having a Māori nurse leader in the Ministry and I suppose the Ministry and the health sector gets a “two-for-one deal,” she laughed.
“Having a bicultural heritage – having grown up with both Dutch and Maori heritage – I feel I’ve grown up with the best of both worlds and bringing an inherent equity focus into the chief nurse role is timely and a great fit.”
She said she had learnt to combine the synergies between her two cultures and her profession and was looking forward to demonstrating how that can work. “Not just from being a Maori nurse but how I can share that understanding with others and other clinicians.”
Broodkoorn graduated as a nurse from one of the last hospital-based training programmes at the former Greenlane Hospital School of Nursing. She has a Master of Health Science (Nursing) with 1st class honours from the University of Auckland. Apart from a variety of clinical nursing roles, she had education roles at MIT and University of Auckland specialising in kawa whakaruruhau (cultural safety) and Te Tiriti o Waitangi training.
From education she progressed into management and leadership roles as the assistant director of nursing Māori with Auckland DHB, managed a Māori health provider service, and had returned home to Hokianga as a community development manager before taking up the Northland DHB director role in 2010.
Excited at new role but also a little sad
Broodkoorn says one of the sad aspects of her move will be the need to step down from some of her current roles that she has loved being part of, including being on the executive of the National Council of Māori Nurses and her role as sponsor lead of Nga Manukura.
“While it’s sad it is also exciting in terms of the added-value I can now provide to the development of the Māori nursing workforce – just now wearing a different pōtae (hat).”
Broodkoorn is looking forward to working with her national nursing organisation colleagues and working with the yet to be announced new chief executive and registrar of the Nursing Council.
“I am excited but also have mixed emotions as every day that goes past is a day closer to my leaving my role here and that does sadden me because I’ve got such an amazing team here. I work with amazing people in Tai Tokerau who are commited to addressing health inequities in Northland which are significant for our population. …No time is a good time to leave but I just feel there is so much more work to do that I would love to be part of. But I will be home again.”
Broodkoorn said her partner and two young adult children are very proud and supportive of her new role. “I couldn’t and wouldn’t be doing it without their support.”
She starts her position on February 11. She will be joining nursing advisors Jane Bodkin, Kathy Glasgow and Ramai Lord and executive assistant Debra Begg in the Office of the Chief Nurse. She was also delighted to hear of the appointment this week of Martin Chadwick, who she has worked with him before, and was looking forward to working with him and chief medical officer in the Ministry’s new clinical cluster.
Bloomfield has said the new Clinical Cluster, with a combined staff of about 11, will be responsible for contributing strategically to understanding how services can be better planned and delivered including “identifying and promoting innovations at a national level, providing oversight and direction on clinical and professional issues across the sector, and supporting the response to current and future workforce demand”.
]]>Broodkoorn, the current director of nursing and midwifery at Northland DHB, is of Ngāpuhi and Dutch whakapapa and will be the first chief nurse of Māori descent since the forerunner of the role was created nearly a century ago.
Professor Jenny Carryer, executive director of the College of Nurses Aotearoa welcomed the appointment saying she has immense respect for the new chief nurse having worked with her as a former College board member and as a longstanding member of the National Nursing Organisations (NNO) group and NWAG (nursing workforce advisory group). “She is a strong knowledgeable and gracious leader and it is very exciting to see Maori nurse on this core role. She will have the total support of the College.”
Memo Musa, chief executive of the New Zealand Nurses Organisation congratulated Broodkoorn on her appointment and said she would play a vital role in working with NZNO and other nursing and health professional groups to advance and promote nursing’s role in a well-functioning health system.
Te Ao Māramatanga- New Zealand College of Mental Health Nurses were also excited by Broodkoorn being the first Māori chief nurse. “It’s been a long time coming,” said the College’s kaiwhakahaere Chrissy Kake and president Suzette Poole
“Margareth has been integral in supporting our mental health and addiction credentialing programme for primary care nurses in the Northland region,” said the pair. “We look forward to working with Margareth in leading mental health nurses, addiction nurses and disability nurses into the future and continuing to grow the Māori nursing workforce.”
NZNO kaiwhakahaere Kerri Nuku and president Grant Brookes both welcomed Broodkoorn to the role and said they were looking forward to working with her.
Brookes added that the Ministry was operating under a fresh set of priorities this year and he welcomed her appointment as a “bold choice to lead the focus on these priorities”. “I greatly look forward to working with our new chief nursing officer in achieving equity of outcomes and contributing to wellness for all, particularly Maori and Pacific peoples.”
Te Ao Māramatanga welcome
Maranga mai…Takahia te ao ka kitea te iwi e tū tangata mai tātou ngā uri o rātou kua mene ki te pō
Tēnei te mihi ki ngā kai awhina e ki ngā whaea ngā matua anei rā ko ngā hua e puawai ana mai…
As the verse o Ngāpuhi waiata says rise up, make your mark on the world to be seen by all peoples that we [Māori] are people who stand proud, we the descendants of those who have passed onto the night, this is the thanks we give you. To the mothers and fathers, the fruits of your labour blossoming before you.
]]>Ongoing frustration at the pay gap – between nurses working for iwi and Māori health providers and nurses working for other government-funded health providers – saw New Zealand Nurses Organisation (NZNO) representatives speaking out at the Waitangi Tribunal last month about their concerns about pay parity and over institutional racism leading to underfunding of Māori health.
The decision this week by NZNO staff at Ngāti Porou Hauora (NPH) to take strike action is believed to be the first time that any iwi or Māori health provider nurses have taken strike action during the decade-long campaign to close the about 25 per cent pay gap between iwi and district health board nurses.
Kerri Nuku, NZNO’s Kaiwhakahaere, says registered nurses working for NPH earn $14,000 per year less than their colleagues working in district health boards (DHBs) and enrolled nurses working for NPH earn less than HCAs whose wages are covered by the Pay Equity Settlement Act.
Christina Couling, the NZNO organiser, says it was not an easy decision for the nurses to strike with many of them Ngāti Porou themselves who had chosen to continue working for NPH because they wanted to serve their people.
But she says the ongoing low pay had become unsustainable with NPH struggling to recruit new nurses which meant some primary health care clinic nurses were working a full week and then being asked to cover shifts at Te Puia Rural Hospital over the weekend. NPH runs the hospital, (which has a residential aged care facility and 24 hour emergency health services) plus seven primary health clinics in Gisborne and across the East Coast, as well as offering rural/district nursing and mental health nursing services.
NZNO said NPH’s current offer amounts to no more than two percent, with some staff being offered no increase at all. It said last year staff narrowly voted to accept a zero percent pay increase but now say they have had enough of being poorly paid and want to be treated fairly and with the respect they deserve.
NPH has been contacted for comment by Nursing Review but had yet to respond. It is understood that the parties will go to mediation on Monday.
Rural health nurse Gina Chaffey-Aupouri (Ngāti Porou) said NPH nurses and health care assistants were caring people who were key to addressing the incredibly high health needs in the area.
“We just want to be paid the same as our colleagues working down the road who have the same qualifications and experience as we do,” she says.
“It’s just not fair to anybody. We already face so many barriers because we’re away from the main centres and we just can’t attract new staff when they can earn so much more working elsewhere. So we carry on, and we do the extra hours because we’re understaffed. We love and care for our people, but enough is enough and somebody has to stop and listen.”
Couling said the four unions involved (NZNO, the PSA, FIRST and E tū) want a fair pay increase for their members and a plan from NPH about how it will address stagnating wages and pay inequities between these and other nurses. No plan has been forthcoming despite negotiations having taken place for nearly a year.
“What we have here is another clear case of inequity and underinvestment in rural communities that have a significant proportion of Māori, and people in poverty with high health needs,” she says
“It’s fundamentally unjust when a DHB will not give its health providers the funding required to pay nurses at the same rate as nurses working in DHBs – despite them having the same qualifications, expertise and importance. It should not be left to hard-working, dedicated nurses to bear the brunt when finances are tight.”
]]>The appointment of Tracy (Tūhoe, Whakatōhea and Ngāti Kahungunu) – who is in her second year of nursing study at Te Whare Wānanga o Awanuiārangi in Whakatāne – has come at a pivotal time for Māori nursing.
A more than decade long campaign to close the 25 per cent pay gap faced by nurses working for underfunded Māori and iwi health providers compared to their DHB colleagues is in front of the Waitangi Tribunal.
Māori nurses are to share their frustration and argue that the Crown’s failure to address the pay disparity – despite repeated submissions on inequitable funding – is evidence of institutional racism in the health sector. Also pointing to the ongoing gap in health outcomes betweenMāori and non-Māori and the need to boost the Māori nursing workforce as an important step to help reduce the disparity.
 “Like it or not we are the future of nursing,” says the new student leader. “Only a few hours
“Like it or not we are the future of nursing,” says the new student leader. “Only a few hours
after I was elected Kaiwhakahaere Kerri Nuku organised myself and another to talk to two Ministry of Health representatives aboutissues that students faced, one which is what can be done to train more Māori nurses and then retain them. We will be going to talk to them again in Wellington soon.”
Whānau heartbreak
Tracy’s journey to studying nursing has been, at times, arduous. “I’ve seen first-hand the barriers Māori are faced with, when in hospital. My dad passed away recently (due to cardiac issues). He was my biggest supporter. I’ve met with some personal challenges on the way to achieving my dream of becoming a Māori registered nurse, but I know he will always be with me spiritually.
“Kei te hotuhotu te ngākau mou pāpā, a tonā wa ka tutaki taua ano. Moe mai ra toku pāpā I roto I ngā ringaringa o te Atua”
Her son was diagnosed with rheumatic heart fever at the age of 12 and Tracy spent three months at Starship Hospital with her boy.
“That’s where I saw how amazing nurses are. I didn’t know anything and they were so calm sitting day after day with us explaining what was happening.”
Tragedy struck again when three years ago, Tracy’s brother passed away from cardiac issues when he was aged just 41.
“It was the final push I needed. I decided then and there, that I didn’t want any more whānau to pass away from illnesses that are preventable and treatable. If I can prevent one whānau from going through the heartache my whānau has been through, this would be worth more than any amount of money anyone could give me.
Inspired to study nursing
“I knew if I wanted to help my whānau I needed to get educated. When I looked into the possibility of studying again it was quite daunting because I was an older student, I had limited knowledge of anatomy and physiology, and it had been a few years since I’d left high school.”
Tracy began a Te Reo Māori course at Te Whare Wānanga o Awanuiārangi in 2015.
“That gave me the grounding and confidence to progress to the half-year bridging programme to nursing in 2016. I started in Te Ōhanga Mataora Paetahi – Bachelor in Heath Science Māori Nursing – in 2017.
“At my instituition Te Reo Me Ona Tikanga is a living, breathing part of our nursing journey it is just as important as the clinical skills we learn. Cultural and clinical competences are interwoven into our curriculum and are designed to ‘inhibit’ differences in ethnicity, this is the point of difference that our programme offers.
“Another key part of our programme as tauira (students) we are not just an ID number; we are real people who can talk and engage with our lecturers if we need any support whether it’s academic, pastoral care, clinical support or just someone to confide in.”
Cultural dimension
She says she looks at things from a Māori lens – rather than from an outsider looking in at Māori. She says this is partly why Māori patients and their whānau respond differently to Māori nurses.
“Recently at a hospital, a Māori patient wouldn’t touch their food. When I came in I saw there was a urine bottle near where their food sat. It was that easy and that profound.”
Perhaps unlike many of those who step into more political roles, Tracy said she does not see herself as a leader. After people pointed it out she realised that people listened (to her) but it was with “a lot of encouragement” she “hesitantly” put her name forward.
“I have a strong voice that I can use to support and advocate for students. Prior to the election, I had been attending hui in Tauranga for Te Rūnanga, I sat and listened to, and was inspired by, Māori registered nurses encouraging and inspiring students to keep pursuing their dreams to become registered nurses.”
Tracy is passionate about providing cultural support for nursing students.
“At the recent student hui a tau, multiple issues of concern were identified. One of those voiced was the withdrawal of/limited cultural support/services available to nursing tauira.
“I am reluctant to identify the schools that have removed cultural services as this could possibly affect the tauira that raised the issue. I can confim that only five nursing schools identifed that they have strong cultural support within their institutions.
“Tauira also identified another eight nursing schools where the cultural services offered were limited, or in fact, non-existent. I was saddened when one tauira said: ‘If cultural services were to be removed no one would notice a difference’. It made me realise that the services we are offered at my instituition are not the norm.”
“Chairing Te Rūnanga Tauira gives me the opportunity to support and advocate for nursing students to make a positive change. I have been able to listen and speak to delegates across the country to gather their views as Māori student nurses. I carry these views when I campaign, to make changes.”
And the mother of four says that while her life experiences saw her dream about being a cardiac nurse, her dream now is to be a Māori registered nurse.
“I know the rest will fall into place from there. Where my people need me is where I’ll go.”
*NZNO’s National Student Unit has two parts – the National Student Representatives (NSR) and Te Rūnanga Tauira (TRT). Dion Reid is Chair of the NSR and Tracy is Chair of TRT.
]]>Māori nurses are to share their frustration and argue that the Crown’s failure to address the pay disparity – despite repeated submissions on inequitable funding – is evidence of institutional racism in the health sector.
The nurses will be speaking up in support of the Wai 2713 claim made by NZNO Kaiwhakahaere Kerri Nuku and Hineraumoa Te Apatu on behalf of the Te Rūnanga o Aotearoa of Tōpūtanga Tapuhi Kaitiaki o Aotearoa (NZNO). Their evidence will follow the two claims by two Māori and iwi health provider groups who started giving evidence on their similar funding and institutional racism grievances at the start of the historical Waitangi Tribunal hearing at Tūrangawaewae Marae this week
The nurses and providers claims are part of the global Wai 2575 Health Services and Outcomes Inquiry that groups together the more than 200 individual and group claims seeking the Crown to address a wide range of health-related grievances that are broken into three stages – the first focusing on primary health.
Nuku has twice taken the case for Māori nurses to the United Nations after saying “enough is enough” following the failure of the long-running Te Rau Kōkiri campaign for pay equity for Māori and iwi provider nurses that has been ongoing since the DHB ‘pay jolt’ of 2005 created a pay gap that continues to grow.
A petition was presented to Parliament in 2008 calling for the Government to work with NZNO and the providers so that pay equity could be funded but a Health Select Committee recommendation to look into the petition issues was vetoed by the Government in 2009. The Rūnanga has also raised the issue at International Labour Organisation forums and lobbied and met with the Human Rights Commission, Ministry of Health and four health ministers.
“No one within the New Zealand government is listening, despite the fact that we have raised this issue numerous times,” says Nuku in her evidence statement filed with the Tribunal. “This is why we have had to take such expensive and dramatic methods (i.e. presenting at UN).”
Their claim says the pay disparities – which will increase with the recent DHB nurses pay settlement – are a by-product of how the Crown funds the Māori and iwi providers differently from general practices belonging to large primary health organisations. They say the funding fails to address the differences in infrastructure investment required for Māori versus other larger health providers. Also that funding contracts awarded to Māori providers did not allow for pay equity nor recognition of the dual competencies of many Māori nurses.
“Each year this issue remains unresolved Māori whānau continue to receive less income than the families of nurses working within district health boards and other parts of the health sector,” says the claim.
One of the Māori health provider claims also point to a 2007 Deloitte Report – prepared in response to an initial Waitangi claim made in 2005 – indicating Māori PHOs and providers were being collectively underfunded by $21.77 million a year and they say nothing has been done by the Crown in the decade since to remedy that underfunding.
The nurses’ claim has three recommendations with the first two being for a systems-change based action plan to eradicate institutional racism across the health sector and for the “detection, prevention and eradication of racism” to be built into all health sector quality assurance systems.
The last asks that “urgent action and leadership be taken by the Minister of Health and/or the Ministry of Health to reconfigure contracting and funding processes to ensure pay parity for nurses working in Māori and iwi health providers with those elsewhere in the health sector”.
The Wai 2575 Health Services and Outcomes Inquiry, primary health claims, are being heard in a series of hearings in October and November at Tūrangawaewae Marae, in December in Wellington and finally in March next year to hear closing submissions. The stage two claims will cover three main areas with the first being mental health (including suicide and self-harm, the second being Māori with disabilities, and the last encompassing issues around alcohol, tobacco, and substance abuse. That stage is expected to begin midway through next year. There is currently no start date for the stage three claims which will cover the remaining national significant issues and eligible historical issues.
]]>The 25-year-old of Ngāti Awa, Tuhoe and Te Arawa descent was announced as joint winner with Annie Stevenson at the annual NZNO awards dinner last night
Ruha-Hiraka now works as a practice nurse at Kawerau Medical Centre, where she had also worked part-time as a healthcare assistant throughout her three-year degree. The majority of the centre’s patients are Māori and the centre nominated their young protégé – who is fluent in te reo – for her passion for improving the health status of Māori through prevention and education, and her work as the centre’s smoking cessation champion with the COPD management programme.
She says that when her boss nominated her she didn’t believe she had a chance of winning as “the calibre of the past winners was so high”. So she was so very excited to find she had won. “I was, like, stoked…I couldn’t believe it! I was so thankful, honoured and proud.”
Ruha-Hiraka grew up with her first language as Māori and said speaking te reo meant she felt she was able to connect and build rapport quite quickly with her Māori patients. “And we do have some kaumātua who struggle to understand consultations done in English so I do some of my consultations in Māori, which is easier for me and for them. So it’s a win-win.”
She says her Te Ōhanga Mataora Paetahi (Bachelor of Health Science Māori Nursing) at the wānanga was amazing, including its holistic focus on using the te whare tapa whā model to make them consider all four sides of Māori health – tinana (physical), wairua (spiritual), whānau (family) and hinengaro (mental) – when working with Māori patients.
“I’ve been brought up with te reo Māori and with the Māori world view, so I have basic knowledge of tikanga and I apply a lot of that into my practice as well. Which I feel our Māori patients appreciate.”
Though originally from the Bay of Plenty, Ruha-Hiraka had full te reo-immersion schooling in Wellington from kohanga reo, kura kaupapa and on to wharekura. A new job saw her nurse mother bring the family home to the Bay of Plenty, where Ruha-Hiraka decided to enrol and be part of the first Whakatane cohort of the wānanga’s kaupapa Māori nursing degree. She gave birth to her daughter Tewaituarangi in her second year but was so determined to finish her degree on time that she went straight back to school the day after giving birth as she had an assessment.
“I just continued my studies with no break,” she says. “I was working part-time as a healthcare assistant, was a full-time mum and did full-time study all at the same time.” “But I couldn’t have done it without my whānau – they were my number one support system. Without them, I don’t think I would have been able to continue that quickly.”
Ruha-Hiraka says after leaving school she had been contemplating medicine but having shifted back to the Bay of Plenty she had been keen to stay there to study. Now midway through her new graduate year, she says she wants to continue studying and is considering starting on the nurse practitioner pathway in her chosen field of primary health care.
But first she is looking to celebrate her win and says as it is her partner’s birthday the day after the awards they might head off with their baby for a weekend away.
At the awards, NZNO kaiwhakahaere Keri Nuku acknowledged Ruha-Hiraka’s use of tikanga and te reo to create a safe and respectful environment when working with patients and their whānau, and said she truly deserves recognition for her hard work and dedication.
“You are a wonderful role model for young and Māori nurses, and we couldn’t agree more with staff at Kawerau Medical Centre, who say they are lucky to have you.”
Runner-up Te Rongopai Clay-Mackay, a young Plunket Nurse working in Porirua, was also acknowledged for her work in improving health for Māori. She is the first Plunket nurse to deliver both Well Child and B4 School programmes in te reo Māori and Nuku said Te Rongopai stood out for being “a vibrant, committed and caring young nurse who has demonstrated an incredible amount of maturity and professionalism in her work”.
The 2018 award winners and runners-up were chosen from 14 nominations. The judging panel consisted of representatives from all district health boards, the Office of the Chief Nurse (Ministry of Health), the NZNO President, kaiwhakahaere and nursing staff, and last year’s winner Jess Tiplady.
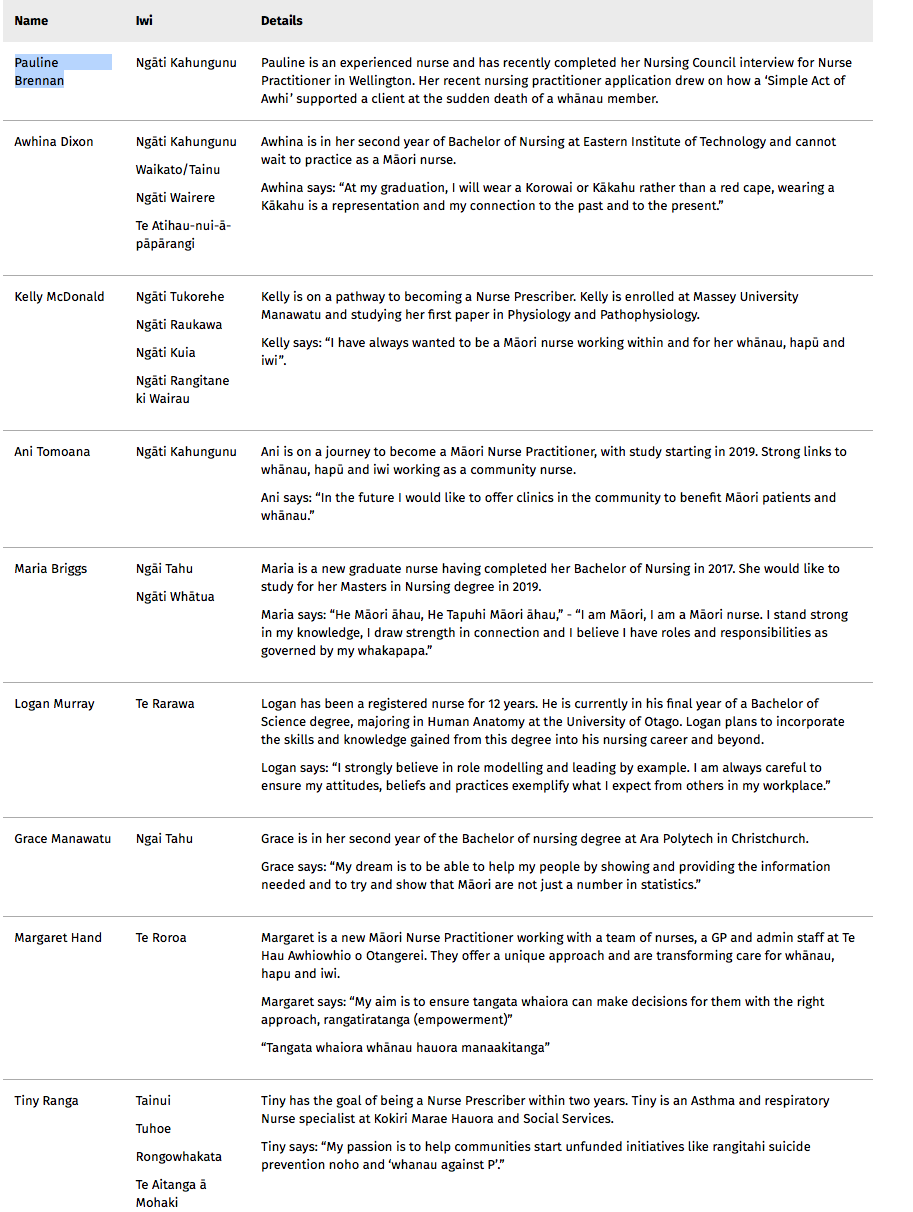
]]>The Tapuhi Kaitiaki Awards recognise Māori nurses who are furthering their studies, clinical practice and professional development while continuing to support the wellbeing of whānau, hapū and iwi.
“Māori nurses play a unique role in the health sector in that they are both clinically and culturally competent health professionals,” said NZNO Kaiwhakahaere Kerri Nuku on the new awards.
Alison Hill, Pharmac’s Director of Engagement and Implementation said a Pharmac goal was eliminate inequities in access to medicines by 2025, and improving Māori health outcomes was a key focus.
“Māori health professionals have a pivotal role in helping Māori understand and access the medicines they need,” said Hill.
“We were really pleased with the quality of the applications, which painted a vivid picture of the deep understanding and strong commitment these nurses have to serving their communities through their profession. I was impressed to see how much these nurses fit into their daily lives, juggling their studies, tamariki, home and professional lives.
She said each of the nine winners demonstrated strong connections and dedication to their whakapapa and community, while continuing to strive towards excellence in their studies or professional practice.
Recipients of the 2018 Tapuhi Kaitiaki awards each received $2000 to $2500.
Dr Jill Clendon, the Ministry of Health acting chief nursing officer, said the Ministry was working closely with the Māori caucus of the National Nursing Organisations on a workforce development programme to help meet the 2028 goal.
The recently released final report for the new graduates who applied through the ACE system in November last year shows that by the end of June just under 86 per cent (85.9%) of the 206 graduates identifying as Māori had gained places in new graduate programmes. This was higher than the overall average employment rate of 82.3% (1124 of the 1357 applicants) but slightly lower than the 88.2% employment rate of the 85 Pacific nursing graduates applying in November last year.
The statistics also showed that Māori applicants made up 15.2 per cent of all applicants and 15.7% of those who gained employment through ACE – or about the same as the Māori population.
But higher numbers will be needed to trained, recruited and retained if the total Māori nursing workforce is to grow to closer to the 15 per cent goal.
Clendon said the Ministry had recently hosted a hui focusing on Māori workforce development involving leaders across the Māori workforce including educators, clinical practice and management.
She said it discussed issues important for the employment of new graduates including “building and sustaining Māori nurses so they feel safe to practice and they are safe to be Māori in those environments”. Also discussed were aspects of kawa whakaruruhau (cultural safety). “Not just about safety of nurses in practice but the safety of Maori nurses to be practising safely as well.”
Clendon said this went back to the original intent of its founder Irihapeti Ramsden which had been “a little diluted over the years” and the Nursing Council was now going to revisit this with the Māori caucus.
She said the Ministry and the caucus will be engaging with Māori students to discuss what concerns they had.
“Although we are seeing some really good figures around our ACE programme. We’ve also heard anecdotally that some Māori student are choosing not to apply through ACE. And we need to be unpicking that and looking more closely to understand why.”
It will also be exploring why some young Māori are getting into the undergraduate programme but not going on to graduate. “We need to understand that if that is happening, why is it happening and what can we do to support that. So they do have opportunities to come out the other end into our NETP [nursing entry to practice] programmes. Then we have to make sure that our NETP programmes are appropriate for Māori nurses.”
Meanwhile the latest ACE statistics show that – after initial disappointment that only 9 of of the Te Whare Wānanga o Awanuiārangi’s first graduating class from its kaupapa Māori nursing degree obtained jobs in the first round – employment had risen to 14 or 77.8% of the 18 applicants included in the ACE match.
The Bay of Plenty DHB, where the wānanga is based, took on the highest number of Māori graduates of any DHB – 24 which was nearly half (47.1%) of the 51 graduates they employed. The next highest was Southern DHB, which took on 17, followed by Waikato with 16, Auckland with 15 and Capital & Coast with 14. The DHB that took the highest proportion of Māori graduates was Tairawhiti, where 9 of the 11 (81.8%) new graduates they employed were Māori, followed by Lakes, where Māori made up 11 of their 21 (52.4%) new graduates taken on.
]]>The New Zealand Nurses Organisation leader is just back from addressing the United Nations Permanent Forum on Indigenous Rights in New York for the third year running to support the case of Māori nurses.
Nuku requested a UN interventionto ensure Māori women’s voices were included in health policy decision-making and for the health system to support having a nursing workforce that matched the Māori population. And on her return to New Zealand has called for the Government’s ‘full commitment” to developing and planning a growing Māori nursing workforce.
“An aspirational Māori nursing workforce goal with no further commitment, funding or implementation strategy is unacceptable,” said Nuku.
In November 2015 the Health Workforce New Zealand’s (HWNZ) Nursing Governance Taskforce for Nursing set a date of 2028 to meet a goal of “significantly increasing” the number of Māori nurses (currently 7%) to better match the proportion of Māori in the population (15.6%), with the aim of improving access to care and the quality of care for Māori.
Nuku said recruitment and recruitment of Māori nurses was vital for the future health and wellbeing of whānau, hapū and iwi and a Maori Nursing Strategy was “urgently needed to address this”.
“Whilst commitment has been made to form some regional partnerships to achieve the goal of a Māori nursing workforce that matches the percentage of Māori in their population by 2028, there is no supporting operational strategy to make this happen.
Health Minister Dr David Clark was unavailable for comment but the Ministry of Health’s acting chief nursing officer Dr Jill Clendon said theNational Nursing Organisations group’s (NNOg)MāoriCaucus – which included Nuku – was providing leadership on developing a strategy to meet the goal, with the support of the Ministry’s Office of the Chief Nursing Officer (OCNO).
“We currently fund a number of operational initiatives to grow and support the widerMāorihealth workforce, including scholarships, cultural support and leadership programmes, and initiatives in secondary schools, undergraduate and post graduate education,” said Clendon. “There are also two Bachelor of Nursing (Māori) programmes based on kaupapa Māori perspectives supporting Māori nurses to work in their communities”.
Nuku also drew attention to the ongoing pay parity issue for nurses working for Māori and iwi health care providers who were paid up to 25 per cent less than their counterparts in district health boards.
An 11,000-plus petition was presented to Parliament back in July 2008, pointing out the inequity and calling for the Government to work with NZNO and Māori and iwi PHC employers so that pay equity could be funded and delivered to their nurses and other health professionals.
“This situation, although complex could be remedied by different contractual arrangements, if there was the political will to do so,” she said. The Ministry said it could not comment, saying DHBs funded Māori and iwi providers to provide primary health care services and that nurses pay was dependent on negotiations between the nurses and their employers.
]]>
Applications opened today (February 14) for the scholarships that are open to Māori students in nine health disciplines including community health workers and health management.
Associate Minister of Health Jenny Salesa said the scholarships were a great opportunity for students and health care workers and offered them support to help them achieve and excel in their chosen health career. She also said enhancing and encouraging Māori representation in the health workforce is hugely important so that the system responds effectively to the needs of Māori.
Currently nurses identifying as Māori make up about seven per cent of the total nursing workforce while Māori comprise about 15 per cent of the New Zealand population. But the percentage of Māori nurses may be on the increase with Māori nurse graduates making up 14-15 per cent of applicants to the latest two rounds of the ACE new graduate job matching process.
There are 11 Hauora Māori scholarship categories (covering nine specific health disciplines plus other undergraduate health-related degrees and Māori students studying towards a postgraduate qualification). There are also three special award categories: the Excellence Awards, the John McLeod Award and Te Apa Māreikura Award. The scholarships and awards range in value from $1000 to $10,000 each. Nursing scholarships are worth $1700 each.
To be eligible for a Hauora Māori Scholarship, applicants must be a student enrolled and attending a university, polytechnic, wānanga or private training establishment based in New Zealand and have whakapapa and/or cultural links with Te Ao Māori or Māori communities.
They must demonstrate a commitment to and/or competence in Māori health and wellbeing and be studying a health or disability-related, NZQA accredited course.
Online applications open at 5pm today (14 February) and close on 28 March.
More details are available on the Ministry of Health website: http://www.health.govt.nz/our-work/populations/maori-health/hauora-maori-scholarships-2018
]]>