This backs ongoing calls by the national nursing organisations for 100 per cent placement of new graduates in new graduate programmes – a goal they had set to be met by this year.
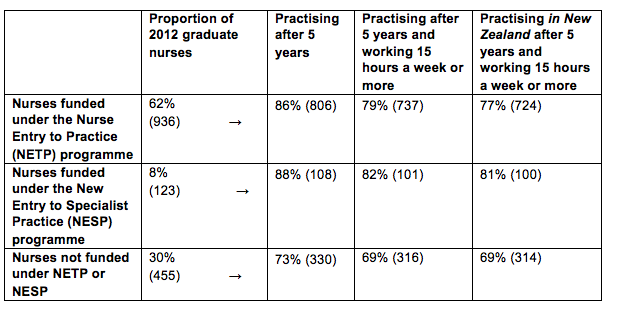
The Ministry of Health analysis found that 86 per cent (806) of the 2012 nurse graduates who gained a place in a government-subsidised NETP (Nurse Entry to Practice) programmes were still in nursing five years on.
The proportion was even higher for mental health nurses with 88 per cent of the 123 new grads signed up to a specialist mental health NESP (New Entry to Specialist Practice) Programme) still having valid annual practising certificates (APC) five years later.
In comparison just 73 per cent (330) of the 455 new graduates who failed to gain a place in a NETP or NESP programme still had an APC in 2017. Overall 1244 (82%) of the 1514 nurse graduates registered in 2012 were still in nursing five years later. (See table below)
Chief Nurse Jane O’Malley said the higher proportion of new graduates still nursing if they had started their careers in a funded new graduate programme was “telling” and showed the importance of the programmes for nursing retention.
In 2013 the National Nursing Organisations – including the New Zealand Nurses Organisation and College of Nurses Aotearoa – called for full utilisation of all NETP funding to support the goal of 100 per cent employment of new graduates by 2018. Government funding is potentially available to subsidise 1300 NETP and about 125 NESP places but lack of vacancies and tight budgets – particularly at district health boards – means only all the NESP funding is fully utilised.
New graduate nurses employed under a year-long NETP programme must receive clinical preceptor support for the duration of the programme and the equivalent of 12 study days with the aim of new nurses starting their career “well supported, safe, skilled and confident in their clinical practice”.
The analysis of the 2012 new graduate cohort – that uses data from the ACE new graduate placement and Nursing Council of New Zealand annual practising certificate data – also showed the vast majority of the new nurses still holding APCs were practising for more than 15 hours a week. (NB nurses practising for less than 15 hours a week but still with valid APCs may be on parental leave, travelling overseas or between jobs.)
The APC data indicated that just over a dozen nurses with valid New Zealand APCs were currently practising overseas. (Retaining an NZ APC indicates that they may only be working overseas for a limited amount of time and/or wanted to retain the option of returning to New Zealand to nurse.)
]]>
From today for the first time nurse practitioners can issue the death certificate for patients in their care. Suitably qualified nurses can also write sick leave certificates.
Dr Michal Boyd, a long-standing NP, says being unable up until today to complete death certificates for patients in her care meant the risk of unnecessary delays and distress for a grieving family.
“As the primary healthcare provider I know the person’s medical conditions and have often led their care over months or even years,” said Boyd. “Now I am able to provide all the care needed for the older person and their family.”
More than a decade in the making, the Health Practitioners (Replacement of Statutory References to Medical Practitioners) Bill was passed in late 2016 but the changes made only come into effect today (January 31).
The Bill amended eight Acts to replace references to ‘doctors’ or ‘medical practitioners’ where nurse practitioners (NPs), and other health practitioners like pharmacists, registered nurses and physiotherapists are now qualified to carry out those roles.
Lobbying began early in the millennium by nurse leaders to identify and remove a range of legislative barriers to nurse practitioners’ practice and formal work began back in 2005 to go through legislation with a fine tooth comb to find references to “doctors” or “medical practitioners” in roles that now could be done by other suitably qualified health practitioners. The acts remove the anomaly where NPs could sign ACC forms and sickness benefit forms but could not sign an ordinary sick leave certificate for work under the Holiday’s Act.
Boyd, a former chair of Nurse Practitioners New Zealand (NPNZ), said today’s enacting of the new laws represented to her the removal of some of the last barriers to being able to practice at the top of her scope as a nurse practitioner.
The Ministry of Health’s outgoing chief nursing officer Jane O’Malley described the passing of the bill in 2016 as the “culmination of years of work” from the nursing sector, the Ministry of Health and other agencies.
Memo Musa, the chief executive of the New Zealand Nurses Organisation congratulated all those involved in the watershed changes particularly the Nursing Council and the Office of the Chief Nurse.
Musa said the amended Acts meant more nurses could improve public access to some medicines and also enable them to work to the full breadth and scope of their practice. “It is often easier and quicker to see a nurse than a doctor so this change means more people in the community can benefit by accessing health care sooner.”
2018 LEGISLATION CHANGES SUMMARY
- Changes across eight Acts amend references to medical practitioners to include health practitioners including nurse practitioners, registered nurses and, in one instance, pharmacist prescribers.
- Seven of the amendment Acts with their new terminology will commence on 31 January 2018 and the Transport Amendment Act will commence on 8 November 2018.
- The amendments enable competent health practitioners (as defined under the Health Practitioners Competence Assurance Act 2003or HPCA Act) working within their prescribed scope of practice (e.g. registered nurses) to carry out new roles as defined by the amended Acts.
- This does not mean that all health practitioners regulated under the HPCA Act will be able to undertake all the amended statutory functions.
- The Ministries of: Health; Transport; Business, Innovation and Employment; and Social Development are responsible for the affected legislation. Other agencies, including ACC and the New Zealand Police, will also need to implement the changes.
AMENDED ACTS
Holidays Act 2003: Health practitioners will be able to certify proof of sickness or injury including suitably qualified registered nurses, if their employer and the Nursing Council of New Zealand recognise that they are competent and safe to do so
Burial and Cremation Act 1964: Nurse practitioners will be able to issue certificates for the cause of death for patients in their care.
Medicines Act 1981: Nurse practitioners will be able to supervise designated prescribers (such as authorised registered nurse prescribers or RN prescriber candidates).
Mental Health (Compulsory Assessment and Treatment) Act 1992: Nurse practitioners, or registered nurses working in mental health, will be allowed to complete a health practitioner certificate for applications for assessment under the Act. An NP will also be able to conduct an assessment examination if approved by the Director of Mental Health. The Director can delegate this approval to the Director of Area Mental Health Service.
Accident Compensation Act 2001: Health practitioners providing treatment to a client will be given the opportunity to participate in preparing clients’ individual rehabilitation plans. Suitably qualified health practitioners will also be able to prescribe aids and appliances.
Oranga Tamariki Act 1989 (formerly the Children, Young Persons, and Their Families Act 1989): Health practitioners will be able to carry out medical examinations ordered by the court when considering whether children or young people have been abused, if the court considers that these health practitioners are qualified for that purpose. In addition, a social worker will be able to ask for medical examinations to be completed by health practitioners qualified for that purpose.
Misuse of Drugs Act 1975: Nurse practitioners, registered nurses working in addiction services and pharmacist prescribers will be allowed to prescribe controlled drugs for the purposes of treating addiction.
Land Transport Act 1998: Health practitioners will be able to request blood tests from drivers and assess and report on their fitness to drive. It will be illegal for someone to refuse a blood test from a health practitioner. Other amendments enable health practitioners to take blood, handle evidential specimens and appear in court to give evidence.
]]>O’Malley, who has been Chief Nursing Officer for seven years, is to become Plunket’s first Chief Nurse in March, in a role reporting to Plunket chief executive Amanda Malu.
O’Malley said it was a coincidence and “unfortunate timing” that her announcement followed shortly after Director General Chai Chuah’s resignation. She added that she had a “great deal of respect for Chai and his vision for the future” and was not leaving because he was leaving. “Sometimes great opportunities come up and you need to grab them with both hands.”
O’Malley said she was very much looking forward to working with the Plunket leadership team on their strategic vision as it was a “perfect fit” with her own health philosophy.
“My belief in the New Zealand Health Strategy – and in particular that we can make better inroads into improving people’s health by paying attention to the early years – is reflected in Plunket’s vision for the first 1000 days of life,” said O’Malley. That it was also a nurse and consumer-led organisation also fitted well. She said she would bring with her to Plunket a wealth of knowledge about how the machinery of Government worked and how policy was developed.
O’Malley said she had mixed feelings about leaving her current role as she had loved her time at the Ministry. Some of the highlights were the coming into effect in January of the long-awaited Health Practitioners (Replacement of Statutory References to Medical Practitioners) Act – which removes legal barriers to nurses and nurse practitioners working at the top of their scope – plus the development with the Nursing Council and NNO (national nursing organisations) Group of the now three levels of nurse prescribing. Also the creation of the ACE new graduate job system which meant there was now a database of new graduate job hunters which had helped employ more new graduates as vacancies arose.
“There are lots of good things to celebrate and time really for me to move on to something new,” said O’Malley.
She said once it was known in the New Year about the appointment of an acting Director General she would be keen to ensure that the Chief Nursing Office position remained at the executive level of the Ministry and reported to the Director General.
“Because nursing is the largest workforce and it is, I believe, the workforce that if better utilised will take us into the mid-Century. So we need a strong leader at the top,” said O’Malley.
Plunket chief executive Amanda Malu said the appointment to O’Malley to the new role recognised the importance of the nursing profession to Plunket.
New Zealand Nurses Organisation Chief Executive Memo Musa acknowledged the hard work Chief Nursing Officer Jane O’Malley had done to increase nursing input into Ministry of Health policy and congratulated her on her new appointment.
Musa said that during Jane’s seven years of service she had overseen an increase of resources at the Ministry to ensure the advice from the nursing profession is effective and timely.
“We want to see more nurses at the top table of policy discussion and development, and there is still more to do to make sure nursing is fully utilised to its full scope in order to care for people, whānau and communities and improve health outcomes,” Musa said.
“We look forward to working with Jane in her role at Plunket as she works to advance and promote the hard work nurses do in their delivery of world class nursing services to mums, whanau and babies.”
Professor Jenny Carryer, executive director of the College of Nurses said O’Malley had been instrumental in ensuring nursing’s contribution to health policy was stronger than it had been “for a long time”.
“The size and positioning of the Office of the Chief Nursing Officer under her leadership has finally been positioned in a way that enables appropriately significant input,” said Carryer. “Jane has worked so hard across so many fronts and her contribution has been huge. Her passion for child health will be well matched in her new position and the College of Nurses wishes her well.”
O’Malley was the director of nursing for the West Coast District Health Board when she was appointed to the Ministry of Health role – then called Chief Nurse – in 2010. She had also been a president of the New Zealand Nurses Organisation (from 2001-2005) and is a former clinical nurse manager and nursing academic.
]]>