This backs ongoing calls by the national nursing organisations for 100 per cent placement of new graduates in new graduate programmes – a goal they had set to be met by this year.
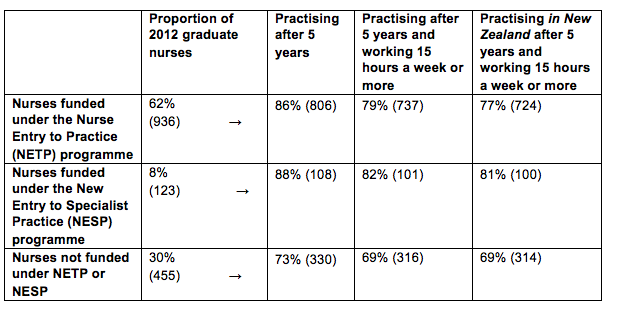
The Ministry of Health analysis found that 86 per cent (806) of the 2012 nurse graduates who gained a place in a government-subsidised NETP (Nurse Entry to Practice) programmes were still in nursing five years on.
The proportion was even higher for mental health nurses with 88 per cent of the 123 new grads signed up to a specialist mental health NESP (New Entry to Specialist Practice) Programme) still having valid annual practising certificates (APC) five years later.
In comparison just 73 per cent (330) of the 455 new graduates who failed to gain a place in a NETP or NESP programme still had an APC in 2017. Overall 1244 (82%) of the 1514 nurse graduates registered in 2012 were still in nursing five years later. (See table below)
Chief Nurse Jane O’Malley said the higher proportion of new graduates still nursing if they had started their careers in a funded new graduate programme was “telling” and showed the importance of the programmes for nursing retention.
In 2013 the National Nursing Organisations – including the New Zealand Nurses Organisation and College of Nurses Aotearoa – called for full utilisation of all NETP funding to support the goal of 100 per cent employment of new graduates by 2018. Government funding is potentially available to subsidise 1300 NETP and about 125 NESP places but lack of vacancies and tight budgets – particularly at district health boards – means only all the NESP funding is fully utilised.
New graduate nurses employed under a year-long NETP programme must receive clinical preceptor support for the duration of the programme and the equivalent of 12 study days with the aim of new nurses starting their career “well supported, safe, skilled and confident in their clinical practice”.
The analysis of the 2012 new graduate cohort – that uses data from the ACE new graduate placement and Nursing Council of New Zealand annual practising certificate data – also showed the vast majority of the new nurses still holding APCs were practising for more than 15 hours a week. (NB nurses practising for less than 15 hours a week but still with valid APCs may be on parental leave, travelling overseas or between jobs.)
The APC data indicated that just over a dozen nurses with valid New Zealand APCs were currently practising overseas. (Retaining an NZ APC indicates that they may only be working overseas for a limited amount of time and/or wanted to retain the option of returning to New Zealand to nurse.)
]]>
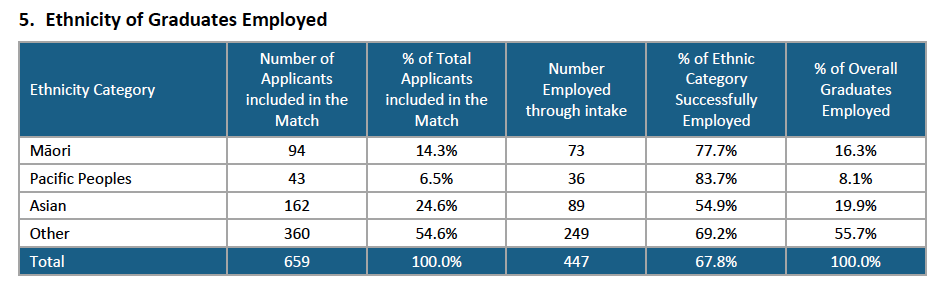
The ACE Nursing Intake Summary Report** for the mid-year intake showed that 447 – just short of 68 per cent of the 659 applicants – received a job offer for a new graduate programme place between July and late October via the ACE job-match process.
When the mid-year pool closed on October 27 there were 190 (28.8%) left in the pool who were still seeking supported new graduate jobs – over a hundred less than the same time last year.
This was the lowest percentage of the mid-year intake still job-hunting into the spring since ACE records began in mid-2013 – and just over a hundred less than the same time last year, when 43 per cent of mid-year applicants were still job-hunting in the spring.
The 51 nurses taken on by mental health and addiction providers for NESP [new entry to specialist practice – mental health and addictions] programmes contributed. The improved mid-year employment rate was also reflected in the findings of the annual mid-year graduate survey undertaken by NETS (Nurse Education in the Tertiary Sector).
According to the ACE report Pacific nurse graduates were proportionately the most successful in getting a job through ACE with 83.7 per cent of the 43 applicants being employed. The next most successful were Māori graduates with 77.7% of the 94 applicants being matched with a job.
The “other” ethnicity category – which includes New Zealanders of European descent – made up just over half of the applicants – 360 (54.6%) and had a job success rate of 69.2%, which was just above the overall job success rate of 67.8 per cent*. Kiwi nurse graduates of Asian ethnicity made up 162 (24.2%) of applicants and had a 54.9% per cent job success rate – the lowest of the four ethnic groupings. (NB to be eligible to apply for a funded NETP [nursing entry to practice] or NESP [new entry to specialist practice – mental health] position through ACE you need to be a New Zealand citizen or hold a permanent/returning resident visa.)
In November 2015 the Health Workforce New Zealand’s (HWNZ) Nursing Governance Taskforce for Nursing set a date of 2028 to meet a goal of significantly increasing the number of Māori nurses so as to better match the proportion of Māori in the population, with the aim of improving access to care and the quality of care for Māori. ACE statistics for the end of 2015 showed 54 per cent of Māori graduates were known to be employed, compared to 50 per cent of non-Maori and 53 per cent of Pacific applicants.
By mid-2016 the Governance Taskforce had consulted and endorsed ‘levers’ to help meet the goal including supporting all Māori new graduates into employment, building on current initiatives to promote nursing careers, and building Mâori faculty at universities and other providers.
The mid-year intake analysis indicate that the push may be paying off but the director of the Wānanga based kaupapa Māori nursing degree, Ngaira Harker, has expressed disappointment at the intial job offers for its first graduate cohort of 19 nurses who are part of the latest end-of-year ACE intake. At the end of November nine had jobs (just under half) which was a lower job rate than the 57 per cent of total applicants who had been offered jobs in the same time period, according to early ACE stats for this latest job match round.
Auckland biggest source of jobs
The cost of living in Auckland didn’t seem to put off new graduates seeking work for the three Auckland district health boards.
Auckland DHB had the highest number of applicants putting it as their first preference (118) and had 312 applicants in total expressing a preference for Auckland as their first, second or third preference. Waitemata DHB was the first, second or third preference of 229 applicants and Counties-Manukau had 200 applicants.
In all there were 260 applicants in the mid-year intake (just under 40 per cent of total applicants) who were graduates from the five nursing schools based in Auckland. The three Auckland DHBs between them took on 199 new graduates (Auckland DHB 87 and the other two 56 each) which was the equivalent of 44.5 per cent of the total jobs on offer nationwide.
The other two largest DHBs, Canterbury and Waikato – also got high interest with 108 graduates putting Waikato as their first preference and 106 putting Canterbury.
Canterbury DHB employed the highest number of new graduates in the country, 91, and Waikato employed 56.
*ACE Nursing mid-year job match round statistics
- 659 applicants took part in the ACE mid-year job match (461 were first time applicants, 169 second-time applicants and 29 were applying for their third round or more.)
- 389 jobs were initially offered by employers (338 NETP and 51 NESP)
- 327 applicants in July were electronically matched and a further 26 manually matched with jobs.
- 346 accepted the job offers (seven applicants failed state finals or declined job offers)
- 101 of the remaining 306 unmatched applicants were offered jobs before the ACE national talent pool closed on October 27.
- 447 (67.8%) of ACE applicants in total were successfully matched with a job.
- That left 190 (28.8%) of applicants still seeking a NETP or NESP placement as at October 27 and a further 22 (3.4%) of applicants had declined offers, failed state exams or withdrawn from the pool.
**The ACE Nursing Intake Summary Report was prepared by agency TAS (formerly known as DHB Shared Services) which owns ACE Nursing on behalf of the 20 DHBs.
NB: This article was corrected on December 22 to clarify that the report was released by TAS rather than the Ministry of Health.
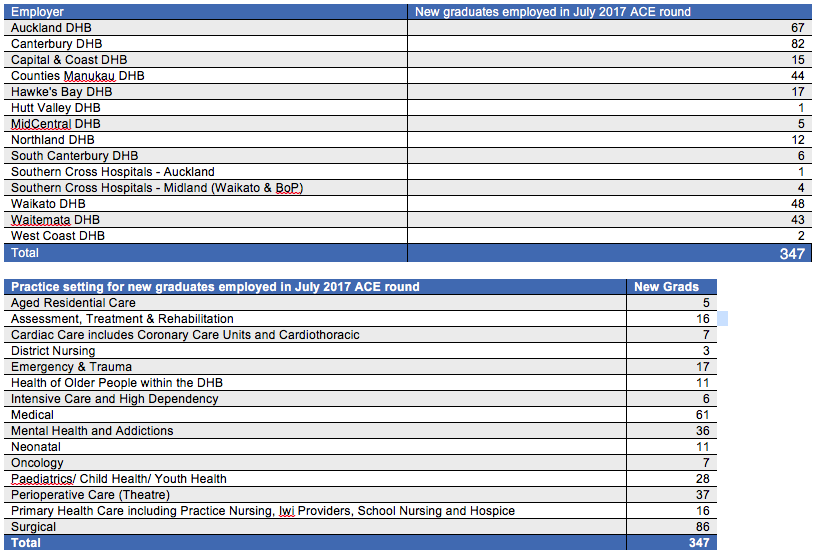
]]>Statistics released by the Ministry of Health showed that 347 of the initial 701* new graduate applicants were matched with jobs in the July round of ACE nurse graduate job clearinghouse. This is equivalent to 49.5 per cent – slightly down on the 53 per cent success rate last year when 332 of 648 applicants were successful.
Nearly 390 positions had been available in the mid-year job round across 12 of the 20 district health boards (see table below) and six positions in two Southern Cross Hospitals – which was up on the 350 jobs on offer at the same time last year.
In the latest round, jobs were initially offered to 354 candidates but seven candidates declined positions or advised ACE that they had failed state finals. But by the end of August a further 48 candidates from the remaining talent pool had been matched with jobs, bringing the number of successful mid-year candidates up to 395 (56.3%) and leaving about 262 applicants still in the job-hunting pool.
Chief Nursing Officer Jane O’Malley said about 600 of the approximately 1800 New Zealand-trained nurses registered each year graduated in July and the goal was for all graduates to be employed. Data gathered since the ACE process began in 2012 found that 40-60 per cent are offered jobs before they have their state final exam results, 60-70 per cent are employed within five months and almost all are employed with 12 months.
O’Malley said in the latest round 251 (60 per cent) of the 421 applicants who had just sat their state finals were offered jobs in the initial round. A further 27 were employed from the talent pool, making a total of 278 (66 per cent) being employed within two months.
The majority of the latest ACE job offers were from across the three DHBs in the Auckland region (154), followed by 82 jobs offered by Canterbury DHB and 48 by Waikato DHB. Surgical (86) and medical (61) were the most common positions filled, followed by perioperative (37) and mental health and addictions (36). (See more details in tables below.)
In total, 466 of 701 initial applicants were applying to ACE for the first time (the 421 July graduates plus 45 graduates from earlier cohorts) and of these 276 (60 per cent) were successful in the first round. This is slightly down on the 62 per cent success rate in the initial round for first time applicants at the same time last year.
Seventy (33 per cent) of the 211 applicants who were applying for jobs through ACE for the second, third or more times were successful in their latest attempts. The ACE data also indicates that 20 (4 per cent) of the graduates from July last year are still seeking new graduate positions through ACE.
*N.B. Forty-four applications were withdrawn prior to the job-matching process, either because they had gained employment or failed to complete their degrees, bringing the total number of applicants taking part in the round down to 657. The same time last year 27 applicants withdrew before the match, bringing application numbers for the match down from 648 to 621.
]]>
But a technical glitch in the ACE nurse graduate job clearinghouse system resulted in 297 applicants who had missed out on jobs incorrectly receiving an email saying they had been offered a job. Also some applicants who had been offered jobs received emails incorrectly stating the DHB they were being offered employment by.
After the error was discovered the ACE Nursing team posted on Facebook at 9.13am yesterday alerting applicants to the error, saying an updated email would be sent shortly and apologising for the inconvenience.
The initial posting prompted 50 comments from graduates and colleagues expressing their disappointment, anger, confusion and frustration at the error.
Comments included one applicant whose response was “Apologies for inconvenience” seriously?? It’s a monumental screw up not a mere inconvenience.”
One poster spoke of spending “one hour on top of the world” believing their third application had been unsuccessful and then being “smacked right across the face” when they discovered it was an error.
Another said they didn’t think “any amount of apology will compensate the ’emotional roller coaster’ that new graduates faced yesterday”. And another: “Apologies will no way make up for the fact these poor grads were celebrating they had a job, then in the next breath they get slapped down abruptly. Gutted for all the new graduates!”
But others were philosophical about the error and one even managed a joke saying, “Phew – I spent 30 mins trying to figure out how I could afford accommodation in Auckland”. (It appears that most or all of the incorrect emails were offering jobs in Auckland.)
An updated posting later that morning from the ACE team said it “extended our sincerest apologies” for the incorrect emails which they said was due to a bug in the email templates in its new IT system and that emails with the correct information would be sent manually.
A press release was issued this afternoon (July 21) in which Julie Patterson, a spokesperson for the 20 DHBs, described the technical error as “most regrettable”.
“We are very sorry that this issue occurred and apologise to everyone affected, particularly those applicants who have not been matched and the distress this may have caused to them and their families,” said Patterson, who is CEO of Whanganui DHB and chair of the DHBs’ Workforce Strategy Group. “We will continue working with applicants regarding their next steps and options such as the talent pool.”
The ACE (advanced choice of employment) clearing house system has been matching nurse graduates and jobs offered through DHBs in the NETP (nurse entry to practice) and NESP (nurse entry to specialty practice) programmes since November 2012 without any previous issues.
Patterson said the error occurred due to the use of a new IT system and that despite checks the “regrettable error” had occurred. “ACE has advised the IT provider that this is completely unacceptable and cannot happen again.”
Applicants who wanted to discuss their individual circumstances were told they were welcome to call the ACE centre on 0800 223 236.
This article was updated at 5.20pm on July 21
]]>
This is the equivalent of 53 per cent of the 648 graduates who applied which is up on the same time last year when 43 per cent of the 662 applicants were successful.*
This latest round saw job applicants slightly down on the previous year while total jobs on offer were up from 285 last year to 350 this year. Not all jobs on offer in government-subsidised NETP (nursing entry to practice) programmes were filled in the latest round but the 18 unfilled positions are expected to be filled shortly bringing the percentage of successful applicants up to a potential 56 per cent.
Of the 441 first time applicants, that is graduates who sat state finals this month, nearly 62 per cent were successful in getting jobs which was up on the 53 per cent success rate last year.
Graduates from November last year made up 174 of the July round applicants with 53 being successful in their second attempt which leaves 10 per cent of the November 2015 graduates still actively seeking work through the ACE system eight months after graduating.
The Ministry said this was a similar pattern to previous years and it anticipated employers would continue to employ graduates as vacancies arose.
Of the 27 applicants applying for the third time six were offered jobs leaving 4% of last year’s July 2015 applicants still seeking work through ACE 12 months after graduating. There were also six applicants applying for the fourth time and it is understood one of those was successful in this round.
*NB 27 applications were withdrawn prior to the job matching process; either because they gained employment or failed to complete their degree.
(Original article amended at 4.45pm July 21 to add information on application withdrawals)
]]>Nursing Review reported in December that 735 (51%) of all new graduate job applicants in the November round were successful and over the summer this swelled to 852 novice nurses (61%) gaining places in new graduate programmes.
But the Ministry of Health statistics from late February show that 39 per cent of the original 1399 applicants* are still seeking a position in a NETP (nursing entry to practice) government subsidised programme.
The numbers are similar to a year ago when 868 (59%) of applicants were placed in NETP or NESP (mental health) programmes by the end of summer leaving 571 (41%) still vying for any remaining places.
But Chief Nurse Jane O’Malley said historical ACE data showed that after 12 months only about 3 per cent of graduates were still actively seeking work through ACE. She added that most district health boards were continuing to employ new graduate nurses and some are planning additional new graduate intakes in the lead up to the expected winter increase in demand.
Ministry statistics show that 132 (63%) of the 211 Māori applicants got jobs through ACE which the Ministry said was a similar trend from previous years with Māori applicants gaining employment at as slightly higher rate than non-Māori. The success rate was not so high for the 103 Pacific applicants with half (51) getting a new graduate position.
The traditional first job settings for new graduate nurses – surgical and medical wards continue to take the highest numbers with 169 new graduates employed in a surgical setting and 130 in medical. Mental health and addictions was the second highest single practice setting taking 133. These three practice settings were also the three most popular first choices of applicants. The fourth most popular first choice, chosen by 132 applicants, was primary health (covering practice, iwi, school and hospice nursing) but only 51 gained jobs in that setting.
Boost needed for declining aged care workforce
One of the least popular choices was aged residential care (the first choice of 16 applicants) and in total 30 new graduates gained jobs in that sector compared to around 38 at the same time last year.
This year there was no additional funding available to support NETP placements in primary care or aged residential care (ARC) – as there had been in previous years through the Very Low Cost Access (VLCA) scholarships or the NETP ARC funding schemes. But for the first time graduates could apply for NETP places with private surgical hospital provider Southern Cross through ACE and by the end of February Southern Cross had 14 new graduates from the July and November intakes.
O’Malley said Health Workforce New Zealand and the Office of the Chief Nursing Officer have developed a workforce forecasting model that estimates there will be 656 fewer registered nurses working in continuing care elderly by 2025, a 15 percent decline. She said consequently the ARC workforce will be a focus including encouraging more new graduates into the sector and ensuring they are supported in their first year of practice.
]]>
Hutt Valley District Health Board revealed this week that a lack of vacancies and overspend of its nursing staffing budget in the winter flu season will see Hutt Hospital not go ahead with its traditional February intake of around 20-25 nurses. But director of nursing Helen Pocknall said Hutt still intends to try and employ a similar number of graduates in 2016, but spread across the year as vacancies arise.
Elsewhere in the country Auckland District Health Board is increasing its February intake from 89 last year to 112 this year and Waitemata will be taking 86 including 8 in primary health care and 19 in the mental health NESP programme. Counties-Manukau DHB is planning to increase its mental health intake by two to 17 and also plans to increase its NETP intake over last year. Waikato is taking just under 90 in February and expects over the year to increase its intake to 105 as part of an ongoing trend of increasing its new graduate intakes.
Hutt Valley’s neighbouring board, Capital and Coast DHB, will also be increasing its intake. Andrea McCance, director of nursing for CCDHB said applicant numbers were slightly up from 289 last year to 304 this year and it had interviewed 170 applicants. She said the board has 46 ‘ring-fenced’ positions for new graduates, up on 40 last year, as well as 25 NESP positions and six places for midwifery graduates.
Final year nursing students around the country sit their state finals exam on November 17 and the following day, November 18, find out whether they have been successful in gaining a new graduate place through the ACE system. The Nursing Council is expecting around 1373 students to sit state finals, which is slightly down on last year’s 1380 candidates.
Whether the total number of new graduate jobs available nationwide have also plateaued or risen will be clearer after November 18. Around 85 per cent (1202) of this year’s 1429 ACE applicants are first time applicants with the rest being unsuccessful applicants from July 2015, November 2014 and earlier graduate cohorts.) Around 150 plus students sitting state finals have not applied for jobs through ACE for a variety of reasons that may include having already found jobs in the private sector or overseas.
Pocknall said Hutt Valley DHB had employed directly 25 of the 37 new graduates taken on across the DHB region in 2014 and 24 of the 35 employed last year. She said this February intake the DHB’s provider arm will be employing none but it hoped to have 3-5 positions available in the primary and residential aged care sector. Hutt had interviewed graduates for NESP places but Pocknall said these positions would be absorbed by CCDHB as the region’s mental health services were now working collectively. Wairarapa DHB was taking on eight new graduates in 2016, the same as this year.
She said Hutt’s nursing leaders had worked very hard with new chief executive Dr Ashley Bloomfield to try and offer some graduate places in the current application round. “But unfortunately we find ourselves where we are now. Having said that we are absolutely committed to take graduates as vacancies come up.” She said last week it had only one nursing vacancy across the whole DHB. On top of the lack of vacancies this year’s flu season had resulted in a “very high rate” of casual nurses being employed over the winter leading to the nursing budget being overspent.
Pocknall said it had considered ring-fencing new graduate positions and offering 12 month contracts but the skill mix required in its specialty areas, like plastics and burns, meant they were unable to regularly take a large number of new graduates. But the board was considering in the future asking each directorate, rather than each ward, to reserve a number of vacancies each year for new graduates. She believed that Hutt was not alone and that several other DHBs may be taking a lesser number or very few graduates this New Year.
But the country’s largest DHB employer, Auckland DHB, is for the second year running increasing its intakes. Two years ago it only had 56 places on offer in November (which grew to 79 over the summer), last year it had 89 places on offer and this year this has risen again to 112 (94 NETP and 18 NESP).
Auckland’s chief nursing officer Margaret Dotchin said the DHB had been increasing the number of graduates over the last few years and last year had three rather than the usual two intakes. “We intend to take approximately 200 new graduates in 2016.”
Denise Kivell, director of nursing for Counties Manukau DHB said it continued to be committed to a strategy of growing its own nursing workforce including a focus on Maori and Pacific nurses. She says it now offers new graduates 12 month contracts and around 97 per cent of its new graduates move into permanent jobs in their second year with the DHB.
Sue Hayward, director of nursing at Waikato DHB, said its trend was for year-on-year increases in its NETP intakes. “The aim is to continue this trend into 2017 – incremental growth to meet population and work force design needs.”
Both Auckland and Waikato application numbers reflected the overall decline in application numbers nationwide with Auckland having 473 applicants this year compared to 561 last year and Waikato having 250 applicants compared to around 350 the year before.
*Since 2012 nursing graduates apply for government-subsidised new graduate positions through the nursing Advanced Choice of Employment (ACE) system. ACE is the national clearinghouse for NETP and NESP positions in district health boards and other government-funded health services like residential aged care and primary/community health providers. This year for the first time it also includes NETP positions offered with private surgical hospital provider Southern Cross.
NB article updated Nov 12
]]>School leavers these days can go online and check out how their likely income as a nursing graduate compares with those for more than 50 other types of graduate degrees.
The information shared on the Careers
New Zealand website is based on Ministry of Education research that uses tax data to track the income and destination of our young graduates (see more about studies below).
The focus is on young New Zealand graduates, with the aim of helping guide young people, their families and their career advisors to make career choices.
Good news – at first
So what does the potential young nurse find out about nursing’s prospects? And how does graduating with a nursing degree stack up against other degrees?
The good news is that, at least initially, the incomes for young nurse graduates stack up pretty well compared with the average young graduate.
Study lead author Zaneta Park says in general the median earnings for nursing degree graduates are good, particularly in the first five years post-study.
She says median earnings start off higher for nursing graduates than for many of the other bachelor graduates, including those who study computer science, accountancy, law, languages and biological sciences. Even five years after graduation, nurses’ earnings are still relatively high – though by this stage law and accountancy graduates are similar and computer science graduates are now higher.
Six years post-study – not so good
But Park says nurses’ incomes then show an unusual trend by dipping in both the sixth and seventh year after study, with the average income seven years post-study actually being lower than it was four years after graduation. The only other graduate group dozens of degrees examined. experiencing a similar trend are the human welfare studies and services graduates, whose income peaks at six years post-study, then falls.
Graduate in both degrees are overwhelmingly female: 95 per cent of young nurse graduates and 88 per cent of human welfare studies and services graduates.
“Our assumption was that this [dip] may indeed be because graduates who complete a bachelor’s qualification in nursing tend to be female and so six to seven years after graduation tend to be more likely to reduce their hours of work for family care reasons (or otherwise make changes that reduce their earnings; for example, perhaps they are less likely to work overtime, or to be on call),” says Park.
But looking at other careers where a high proportion of graduates are female; for example, teacher education (91 per cent) and radiography (89 per cent), there is no similar fall-off in earnings. “We are not sure why this is the case,” says Park.
Another trend in which nursing stands out from the crowd is the high proportion (69 per cent) of young nurses pursuing further study in their first year after graduation, which is due to the many district health boards that include postgraduate certificates or papers as part of their NETP (nursing entry to practice) programmes.
High number pursuing further study
Because the Ministry of Education assigns each graduate to a single destination category each year (and carrying out any study means graduates are assigned to the ‘further study’ category rather than the ‘employment’ category), this results in a degree of confusion for students and parents when comparing job prospects immediately after graduation. (N.B. In table 1 the figures for ‘in work’ and ‘further study’ have been combined to reflect this anomaly.)
Young nurses carrying out further study are rewarded with the median and top incomes for nurses with a postgraduate certificate or diploma being substantially higher (see table) than for nurses with only a bachelor’s degree. But while the incomes of the top 25 per cent of earners kept steadily growing, the median income for postgraduate qualified young nurses also dipped in the sixth and seventh year.
Young nurses heading offshore
Traditionally leaving New Zealand for an OE (overseas experience) has been a common rite of passage for many young New Zealanders and nurses have been no exception.
But if anyone in the nursing sector was concerned that young nurses made up a disproportionate part of the ‘brain drain’ of young people heading offshore, this is not borne out by this study. It shows that eight per cent of 2008–2009 young nursing graduates (a pool of 1,300) headed overseas straight after graduation, which is lower than the 10 per cent average for all 28,800 young people who graduated at the same time.
The number of young nurses heading overseas continues to grow until it peaks at 29 per cent five years after graduation. It then falls back to 25 per cent overseas by seven years post-study, which is considerably lower than the 31 per cent of all graduates from the same time period who are out of the country.
When it comes to health professionals, the number of nurses overseas seven years post-study is on a par with medical graduates (26 per cent) and substantially less than pharmacy graduates (39 per cent), radiography graduates (35 per cent) or dentistry graduates, with the statistics showing half of young dentists are overseas six years after graduating.
Law (35 per cent), accountancy (37 per cent) and computer science (37 per cent) graduates are also far more likely to be overseas seven years after graduation. Amongst the graduates least likely to be overseas are teacher education graduates, with 17 per cent overseas seven years post-study.
Whether the school leaver contemplating nursing will be influenced by these statistics and findings is not known but current statistics show that nursing is holding its own in the graduate income stakes, well for at least the first five years.
Study details
The studies are based on the anonymised tax and tertiary education data of cohorts of young people who graduated between one and seven years before.
The cut-off for this study was the tax year to the end of March 2012, so the cohort of nurses who were seven years post-study was based on nurses who had graduated in either 2003 or 2004. The nurses who were two years post-study had graduated in 2008 or 2009.
The focus of the studies is on young people, with the cut-off age being 24 years or under for nurses on finishing their degree and 26 years or under on completing a postgraduate certificate.
Both the ‘What young graduates earn when they leave’ study (published online May 2014) and the ‘What young graduates do when they leave’ study (published online June 2014) can be found at www.educationcounts.govt.nz.
Zaneta Park, of the Ministry of Education’s Tertiary Sector Performance Analysis group, was lead author for both studies.
The annual graduate destination survey organised by NETS (Nursing Education in the Tertiary sector) showed that 930 of 1192 graduates surveyed in March were working as registered nurses.
The survey data did not include Auckland University of Technology (AUT) graduates but Ministry of Health data shows that 74 of the 104 AUT graduates had been placed in new graduate programmes bringing the total number of November graduate nurses in in work by March up to 1004 – a recent record.
The positive trend was partly due to a plateauing of students sitting state finals, which peaked at 1323 in November 2013 and dropped slightly to 1277 last year. But the employment rate is still considerably up on the 909 (69 per cent) reporting working as nurses at the same time in last year’s destination survey.
As of mid-March there were 273 November nursing graduates not known to be working. The NETS survey indicated that 28 of those were not looking for nursing work currently, at least 162 were actively seeking work and there was no survey data for the remaining 83. (See related story about new graduates seeking working in categories still open to migrant nurses).
O’Malley said the employment market for new graduates remains competitive but there was an upswing in graduates finding jobs earlier than in previous years. She believed the higher employment rate was largely due to district health boards choosing to replace a greater proportion of their nursing workforce with new graduate nurses.
Ministry statistics show that 798 graduates had been placed in government-subsidised NETP (nursing entry to practice) or NESP (mental health) new graduate programmes in public hospitals or publicly funded health sectors. The most common placement was in public health hospital medical (142) or surgical (153) wards followed by mental health and addictions (116) and perioperative (57).
In the non-DHB sector the highest number of graduates found work in primary health care with 62 working in areas including practice nursing, iwi providers and hospices and the residential aged care sector had provided at least 21 NETP places for graduates.
The NETS survey also picked up nurses working in non-NETP programmes in areas like private surgical hospitals, fertility clinics and two graduates nurses working in registered nurse/health care assistant roles in residential aged care.
Cathy Andrew, head of Christchurch’s CPIT nursing school and NETS spokesperson believed this year’s survey results showing 80 per cent employment by mid-March was an “optimistic trend”.
“I think it’s also reflective of the huge amount of effort that has gone into addressing this. Having learnt from the lessons of the past when new graduates haven’t got jobs and they have been lost from nursing and there’s been a crisis a few years later. So there have been initiatives throughout the country where the health sector has gone to significant lengths to make sure they do have vacancies for new nurses.”
She said graduate numbers had increased this decade as nursing schools deliberately increased intakes because of concerns about long-term nursing shortages but schools had plateaued intakes when jobs got a lot tighter around 2012. Andrew also said her own school had noticed a decline in interest in nursing with a hundred less applications for its New Year intake.
The survey also showed fewer graduate nurses heading overseas for work which is part of a consistent trend with graduates nursing overseas falling from 38 in 2013, 24 in 2014 and down to just 12 in 2015.
How many November graduates were still actively seeking work in May would be known presently as applications have just closed for mid-year NETP programme intakes.
Andrew said of the 42 international graduates (that are ineligible for NETP places as they are not New Zealand residents) about half had found work in New Zealand as registered nurses in sectors like residential aged care.
]]>The Ministry of Health has now released statistics showing that in mid-March, 261 graduates were still seeking a job in one of the registered nurse practice settings currently listed on Immigration New Zealand’s long term or immediate skills shortage lists. More than 185 of these nurses had graduated in November with the remaining 75 having been in the job market for much longer.
Immigration New Zealand late last year came out against closing the door to overseas nurses in the areas of medical, perioperative and critical care & emergency nursing after reviewing demand for registered nurses in these practice areas.
Instead it raised the entry bar for migrant nurses from having three years relevant experience to five years experience in the practice area. No changes were made to the entry criteria for overseas aged care nurses wanting to work in New Zealand with Immigration New Zealand saying that it had been advised there was currently a shortage of registered nurses in aged care.
Nearly 1000 visas were issued to aged care nurses (438 on essential skill visas and 555 skilled migrant visas) in the 12 months to May 31 2014. Visas issued for the other three categories ranged from 29 for perioperative nurses to 116 for medical nurses.
Statistics from the Ministry of Health’s ACE job placement clearinghouse, shows that 142 new nurses had successfully gained Nursing Entry to Practice (NETP) programme jobs in medical ward settings and 57 in perioperative care settings
Immigration New Zealand has once again sought nominations from industry stakeholder on which occupations and job categories should be added or removed from the Essential Skills in Demand Lists in 2015.
The occupations selected for review during 2015 will be announced mid-way through the year
]]>