Many New Zealand general practices – crucial for schooling junior doctors – are at training capacity, a new research study has found.
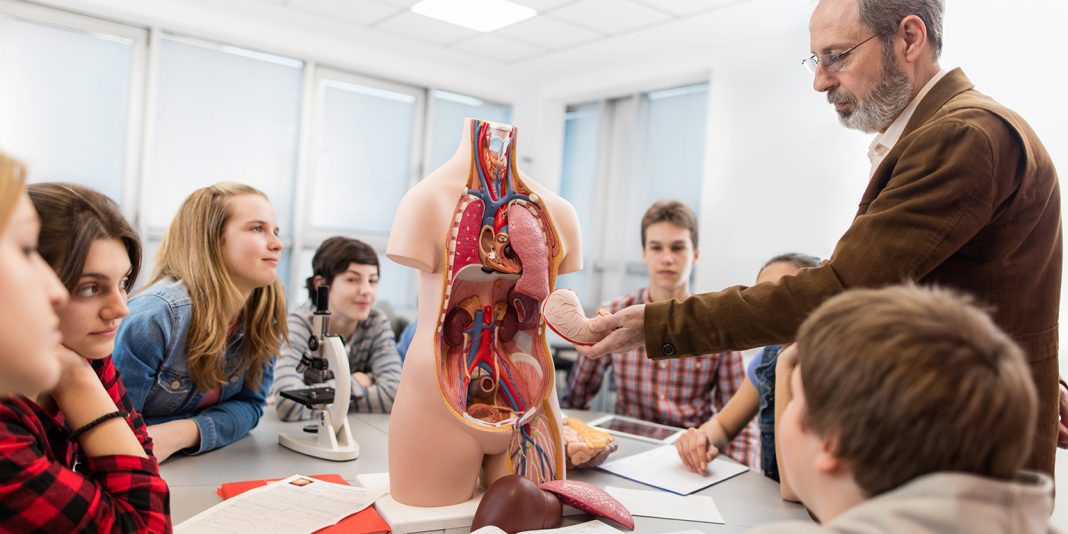
On top of placement as undergraduates, since 2014, junior doctors have been required to take three-month stints in community-focused service, which is most often undertaken in general practice.
The research found that most general practices surveyed in the lower North Island and South Island were already involved in training doctors, nurses and other health care professionals. Most of the training GP clinics undertook was for medical trainees.
Two papers in today’s New Zealand Medical Journal have found 86 per cent of the practices surveyed in the lower North Island and South Island took at least one type of medical trainee, but in a comparable survey undertaken in northern New Zealand, the figure dropped to only 40 per cent.
The study of the lower North Island and South Island, led by Otago University researchers, found GPs needed more support to take more trainees as the current system was poorly co-ordinated.
Further, more were interested in taking junior doctors than undergraduate medical students.
The study of northern New Zealand, led by the University of Auckland, suggested that about 70 practices needed to start taking trainees by 2020 to meet demand, and that the proposed School of Rural Health will help with capacity issues.
“GPs and practice staff say there is little space at present for increasing numbers of trainees in practices,” Otago University researcher Dr Samantha Murton said of the clinics her team surveyed.
“In the future, under the current system, they say they would have to reduce the number of undergraduate trainees if they are going to take on more of those who are in a postgraduate or vocational training position [junior doctors and GP registrars],” she said.
It came at a time when there was increasing numbers of students in both medical schools, increasing numbers of postgraduate and vocational trainees and reducing numbers of GPs to supervise due to the ageing GP workforce.
“High quality primary care is an essential and pivotal part of New Zealand’s health system, and adequate training in primary care settings, for any health professional, is essential to support the present and future health of all New Zealanders.
“To resolve the training capacity issue, three key things are needed – robust and equitable co-ordination between all agencies involved in placing trainees, more training and support for teaching staff at practices, and for smaller practices, help to build additional consultation rooms,” co-author Professor Sue Pullon said.
“To achieve that we need a co-ordinated effort across the training system.”
Murton added: “The survey results suggest that there also needs to be support for teaching in different ways, which will help to make more room for quality teaching in general practice.”