CLINICAL BOTTOM LINE
Low-dose oxygen for patients who have had an acute stroke – but haven’t got severe hypoxia – is safe. But it doesn’t reduce disability or other stroke-related outcomes, indicating that routine oxygen supplementation is not necessary unless needed for other reasons.
CLINICAL SCENARIO
You work on a medical unit where low-dose oxygen is given routinely to patients after acute stroke. This practice is thought to reduce neurological damage and long-term disability. However, you wonder whether it is necessary for all patients and decide to review the evidence.
QUESTION
In patients with acute stroke – for whom oxygen is otherwise not indicated – does routine oxygen supplementation reduce stroke-related disability compared with no supplementation?
SEARCH STRATEGY
PubMed Clinical Queries (therapy, broad): acute stroke AND oxygen supplementation.
CITATION
Roffe C, Nevatte T, Bishop J, et al. Routine low-dose continuous or nocturnal oxygen for people with acute stroke: three-arm Stroke Oxygen Supplementation RCT. Health Technol Assess. 2018;22(14):1-88.
STUDY SUMMARY
A three-arm, randomised control trial (RCT) conducted in acute stroke wards in 136 British hospitals from April 2008 to June 2013. Included were adults with a clinical diagnosis of acute stroke within 24 hours of hospital admission and 48 hours of stroke onset. Excluded were definite indications for, or contraindications to, oxygen treatment, or serious life-threatening conditions likely to lead to death within the next 12 months. In total, 8,003 patients were enrolled and then randomised; consent was obtained from either patients (6,991) or relatives (1,012). All participants received standard care including, at physicians’ discretion, oxygen required for reasons other than stroke.
Intervention 1: (n=2,668) Continuous oxygen via nasal cannula (day and night) for three days. Oxygen flow rate was set at three litres per minute (LPM) if baseline oxygen saturation was ≤ 93% or two LPM if baseline saturation > 93%.
Intervention 2: (n =2,667) Nocturnal oxygen via nasal cannula for three consecutive nights (9pm–7am), flow rate as for continuous oxygen group.
Control: (n=2,668 ) No oxygen supplementation during the three days after randomisation.
Primary outcome: Disability assessed by the modified Rankin Scale (mRS) at
90 days.
Secondary outcomes: Neurological improvement (National Institutes of Health Stroke Scale, NIHSS), mortality (day 7); lowest/highest oxygen saturations during the 72-hour treatment period. Mortality, mRS, independence, living at home, Barthel Index, quality of life (European Quality of Life-5 Dimensions) and Nottingham Extended Activities of Daily Living scale at three, six and 12 months.
STUDY VALIDITY
Randomisation – yes, computer-generated; allocation concealment – yes, web-based; complete follow-up – minimal loss in all groups; intention-to-treat (ITT) analysis – yes ; blinding – outcome assessors for postal questionnaires only; equal treatment between groups – appears so; groups similar at baseline – yes. overall impression: high-quality study.
RESULTS
Participants’ mean age was 72 years; 55 per cent were male and 82 per cent had ischaemic strokes. The baseline median Glasgow Coma Scale score was 15 (interquartile range 15-15), mean and median NIHSS scores were 7 and 5 (range 0-34), respectively. Mean oxygen saturation at randomisation was 96.6 per cent in the treatment groups and 96.7 per cent in the control group. Oxygen supplementation (either continuous or nocturnal) did not reduce disability at three months compared with the control group.
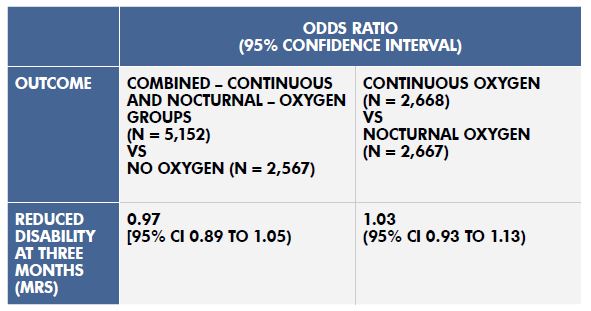
There was no statistically significant difference in disability between the continuous oxygen and the nocturnal oxygen groups (see table). Oxygen supplementation significantly increased oxygen saturation but did not affect any other secondary outcomes. Oxygen had no effect on patients’ levels of disability at any time point, whether given continuously or at night only. Planned subgroup analyses did not detect any benefit on mRS disability score based on risk factors that included stroke severity, baseline oxygen saturation, oxygen treatment before randomisation, time since stroke onset, final diagnosis, GCS score and age.
Table: Results with 95% Confidence Intervals (CI)
Comments
- Large, pragmatic, multicentre RCT. Original sample size calculation of 6,000 patients was revised to 8,000 patients to give greater power to detect an interaction between stroke severity subgroups and the effect of oxygen, compared with control.
- Adverse event rates were similar between groups for the study duration.
- Results do not apply to patients with severe hypoxia (oxygen saturations < 90%) or with indications for oxygen treatment unrelated to stroke. **end bullets**
Reviewer: Cynthia Wensley RN PhD. Honorary Professional Teaching Fellow, University of Auckland [email protected].