LEARNING OBJECTIVES
Reading and reflecting on this article will enable you to:
- Define delirium and the associated clinical features
- Describe the risk factors and causes associated with delirium development
- Identify areas from nursing practice that can influence the detection of delirium
- Understand the role delirium prevention and early identification has in relation to positive client outcomes.
 Delirium is a common and serious clinical syndrome that can occur at any age, but is more prevalent and has greater consequence for older people1. The ageing of the population means delirium is an increasingly prevalent and serious clinical issue that has been likened to a cognitive super bug infiltrating across the sphere of healthcare settings2.
Delirium is a common and serious clinical syndrome that can occur at any age, but is more prevalent and has greater consequence for older people1. The ageing of the population means delirium is an increasingly prevalent and serious clinical issue that has been likened to a cognitive super bug infiltrating across the sphere of healthcare settings2.
Despite the research evidence demonstrating the effectiveness of both primary and secondary prevention strategies, the adoption of delirium best practice as part of routine nursing care has been slow3. While there is a growing awareness of the high prevalence and impact of delirium, clinically, it often remains unrecognised4,5,6, resulting in negative client outcomes. The profession of nursing is well placed to apply evidenced-based knowledge and judgement to assess the health needs and provide appropriate care7 for those at risk or who develop delirium.
Delirium overview
Delirium is defined as a transient mental syndrome that involves a cluster of symptoms that occur together because of physiological imbalances8,9,10,11,12 related to or caused by an underlying medical condition, substance intoxication, or substance withdrawal13.
The characteristic features of delirium include an acute onset and a fluctuating presentation of symptoms, which include disorganised thinking; altered levels of alertness; disorientation; memory impairment; perceptual disturbances (such as hallucinations); sleep-wake cycle alterations; and disturbed psychomotor activity8,9,14.
For most people with delirium, the experience is disturbing and distressing. It is associated with feelings of fear, anxiety, and a sense of being trapped in an incomprehensible situation15.
Nurses report that working with delirious patients can be difficult, stressful, and sometimes dangerous16 and is associated with increased workload and emotional stress15,17. The symptoms of delirium are distressing but the consequences can be dangerous and devastating18. The physiological imbalances that cause delirium can be deadly. Delirium is associated with increased risk of morbidity and mortality, prolonged hospital stays, loss of independence, and residential aged care placement5,10,13,19,20,21. For the older person, delirium can be a catalyst for a spiraling cascade of adverse events that include falls, pressure ulcers, incontinence, and an increased risk of poor functional outcomes10,21,22.
Delirium is particularly prevalent in the acute care environment including surgical, medical, intensive care, and emergency departments6,13. However, it is not confined to the hospital setting alone. Prevalence rates are also high in the residential aged care sector, palliative care services and are on the rise in the home-based community health sector, particularly in people aged 85 years and over6.
Delirium prevention is the most effective strategy for reducing its frequency and complications6 and early detection is essential for improved client outcomes20. As delirium occurs across a number of settings, it falls outside the remit of any one specialty area2, and therefore, there is strong evidence for nurses, regardless of their care setting, to apply evidenced-based principles of delirium prevention, detection and management.
Delirium risk factors
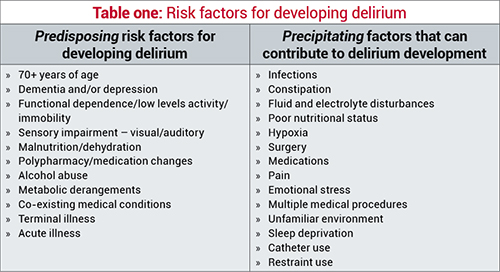
Delirium is a highly predictable occurrence and as such is responsive to primary prevention strategies that include identifying and implementing appropriate care to those at risk2. Many of the risks for developing delirium are highlighted in table one and are divided into predisposing and precipitating factors. Delirium is multifactorial in nature and involves a complex interplay between a vulnerable person, who has predisposing risk factors, coupled with their exposure to precipitating risk factors, which creates a harmful insult6,20,23. For older people, the ability to react and respond to these insults places them at greater risk for delirium as compared to younger people24. Those with high predisposing factors are at greatest risk; however, those without predisposing factors are not immune, especially when exposed to multiple insults. Predisposing factors make the individual more susceptible for delirium, while precipitating factors constitute the direct cause of delirium6.
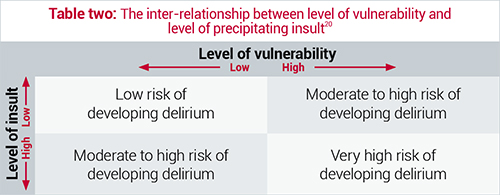
Table two demonstrates how highly vulnerable people, such as those of advanced age, multiple comorbidities and dementia, may develop delirium with only the slightest of insults from a precipitating factor22. In addition, a person without significant predisposing risk factors but who is exposed to multiple insults, such as anesthetics, surgery, catheterisation, and pain and opioid medication, are just as likely to develop a delirium as those with high predisposing factors6,22. In addition, institutional risk factors have also been identified and include number of room changes, absences of a clock or watch, absences of family members, and the use of restraint, either chemical or physical3,25.
Proactive prevention
Knowledge of these risk factors enables nurses to provide proactive and preventative care strategies by firstly identifying people at risk, and then implementing positive care strategies to minimise any modifiable risk factors. Intervention studies based on protocols to assess for delirium risk factors, in conjunction with risk factor modification, have demonstrated a reduction in delirium development3,26,27,28. Nurses can prevent the occurrence of delirium by:
- Recognising those clients most at risk
- Modifying exposure to precipitating factors.
While many of the pre-existing guidelines and literature focus on the acute care setting, several of the modification interventions are applicable across different care settings and include:
- Screening and regular assessment of alertness, attention, orientation thinking, perception, and psychomotor activity
- Orientation to surroundings
- Minimising sensory overload/deprivation
- Providing hearing and visual adaptive devices
- Facilitating nutrition, fluid and sleep
- Promoting mobility
- Including and educating family and caregivers about delirium risks and its clinical presentation.
These nursing-focused interventions can help to minimise the development of delirium but for those that do develop delirium, early identification and prompt management are critical factors for overall prognosis3,20. Despite this, delirium remains poorly detected, diagnosed and managed5.
Difficulties with detecting and diagnosing
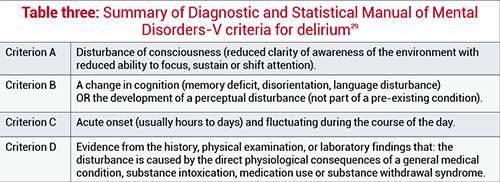
Unlike other medical syndromes, there is no specific diagnostic test for delirium, however, the Diagnostic and Statistical Manual of Mental Disorders (DSM)-V29, outlines the key criteria required for a diagnosis of delirium to be made (see table three). Based on these criteria, diagnosing delirium rests solely on observational and clinical assessment skills that facilitate the identification of the characteristic symptoms1,6. The nurse-client relationship places nurses at the forefront of the diagnosis process, affording them a pivotal role in the detection and secondary prevention of the negative consequences of delirium21,25. However, often the key symptoms of delirium are overlooked by nurses1,18,21, with Inouye and colleagues18 reporting that nurses identified delirium in only 31 per cent of delirious patients.
Comprehensive nursing care includes detailed assessment of clients’ mental status and cognitive function. Commonly used mental status questionnaires such as the Mini Mental State Examination (MMSE) and the more currently used Addenbrooke Cognitive Examination – Revised (ACE-R) are useful tools to support delirium screening and identification. However, these tools do not address the specific symptoms of delirium.
In contrast, the Confusion Assessment Method (CAM) is a well-known validated tool that enables observational assessment of delirium symptoms and is based on the DSM criteria20,23. This CAM enables nurses to more easily detect the symptoms of delirium, monitor clients, and evaluate the effectiveness of management interventions30. The CAM incorporates the features of delirium such as its acute onset and fluctuating course, inattention, disorganised thinking and altered level of consciousness. These characteristic features of delirium should be assessed with any client who presents with an impaired performance on mental status questionnaires12,31.
As with many issues in healthcare, non-detection of delirium is multifactorial. Some key reasons identified relate to the complexity of presentation, limited understanding and knowledge of delirium, and poor attitudes resulting in inadequate communication of symptoms by nursing staff5,32.
In the older population, particularly those with multiple co-morbidities, altered presentation of illness can complicate diagnosis26. Delirium is a complex set of symptoms that fluctuates within a 24-hour period, making it difficult to identify26. Most nurses are familiar with the hallmarks of a hyperactive delirium: heightened arousal, restlessness, agitation, and aggression14. However, often with a hyperactive delirium, it is only detected once a crisis stage has been reached, with the clinical priority focusing on managing the behavioural manifestations and not the underlying cause of the delirium itself12. Not all deliriums present with agitation. Some present with apathy, which is referred to as a hypoactive delirium12,21,33. There is also mixed delirium, which includes features of both a hypoactive and hyperactive presentation.
A hypoactive delirium, which is more common in older people22, is more frequently unrecognised because the behavioural manifestations of drowsiness or withdrawn behaviour do not challenge or disturb others12,34. Those with a hypoactive delirium are perceived as easy to care for and the signs and symptoms of delirium go unnoticed and unreported34.
Ageist assumptions
Nurses can also overlook delirium because they attribute the symptoms as a normal part of the ageing process, with assumptions made that illness and confusion is caused by old age rather than treatable or manageable conditions. Older people with delirium are not only vulnerable to the effects of being unwell but are also susceptible to the misconceptions and ageist attitudes held by nurses8. For older adults experiencing delirium, they can be viewed as a nurse’s burden and an obstacle to effective workload management35. Nurses can treat clients with delirium as if they are experiencing a second childhood and a lack of recognition of the seriousness of the clinical symptoms, but rather, reducing the delirious older person to a process of infantilisation8. Steis and Flick30 found that nurse’s knowledge, recognition, assessment, and documentation of older people differed from that of younger people, with nurses often missing the key symptoms of delirium in older people. It is essential for nurses to explore the impact their attitudes towards older adults and confusion in older adults have on their practice24.
Delirium and dementia
Another common problem for nurses in the identification of delirium is the strong interrelationship between delirium and dementia6. Dementia is a chronic and gradual decline in cognitive function. However, some symptoms can mimic delirium12 and are associated with an increased risk of developing delirium23,26. It can be extremely difficult to identify delirium that is superimposed on dementia as the boundaries between the two conditions are blurred1 and distinguishing between the two is a common clinical problem26. It is not uncommon for nurses to assume and attribute delirium symptoms as dementia, either in those with a delirium superimposed on dementia or those who present with confusion related to delirium34,36. It is critical that nurses identify subtle cognitive changes in a person with dementia that might indicate the presence of delirium12,37. The key distinguishing features between delirium and dementia include:
- Onset: delirium is an acute decline whereas dementia is a gradual decline in cognitive function (island health)
- Fluctuating course: delirium symptoms fluctuate through the course of the day whereas dementia is more constant
- Inattention: in delirium this is a key feature whereas for people with dementia they can pay attention until very late in the disease process.
Conclusion
A high index of suspicion for delirium is needed23,33, with the safest clinical approach being to consider all people who present with confusion as having delirium until proven otherwise26,28. As part of the nursing assessment process, discussion with family/significant others is vital in supporting a diagnosis of delirium by determining baseline cognitive status and recent changes37.When delirium is detected, the key steps in management are to address all evident causes6,10,14. Supportive care interventions aimed at restoring physiological imbalances and preventing further imbalances are vital, as are re-orientation strategies19.
Prevention and early recognition of delirium are paramount to quality care provision and positive patient outcomes. Across all care settings, nurses require an understanding of delirium, its causes and symptoms, and how and why it remains overlooked and under-detected. Many nurses and clinical areas have risen to the delirium challenge and established local policies and guidelines about prevention, identification and management. What have you done to ensure you have the knowledge, skills, and attitudes to prepare you for this epidemic?
Download the learning activity here>>
About the author:
Lisa Stewart RN, BA, PGDipHSc MNur (Hons) is a Professional Teaching Fellow and PhD candidate at the
School of Nursing, University of Auckland.
This article was peer reviewed by:
Stephen Neville RN PhD FCNA (NZ) Associate Head & Director of Postgraduate Programmes, Massey University School of Nursing, Auckland.
Kate Gibb RN PGDip (gerontology nursing) Nursing Director Older People at
Canterbury District Health Board.
REFERENCES
1. MEAGHER DJ (2001). Delirium: optimising management. BMJ 322(7279) 144-9.
2. O’HANLON S, O’REGAN N, MACLULLICH AMJ, CULLEN W, DUNNE C, EXTON C, et al. (2014). Improving delirium care through early intervention: from bench to bedside to boardroom. Journal of Neurology, Neurosurgery & Psychiatry 85(2) 207-13.
3. YOUNG J, LEENTJENS A, GEORGE J, OLOFSSON B, GUSTAFSON Y (2008) Systematic approaches to the prevention and management of patients with delirium. Journal of psychosomatic research 65(3) 267-72.
4. YANAMADALA M, WIELAND D, HEFLIN M (2013). Educational Interventions to Improve Recognition of Delirium: A Systematic Review. Journal of the American Geriatrics Society 61(11) 1983-93.
5. RIGNEY T (2006) Delirium in the hospitalized elder and recommendations for practice. Geriatric Nursing 27(3) 151-7.
6. INOUYE S (2006). Delirium in older persons. New England Journal of Medicine 354(11) 1157-65.
7. NURSING COUNCIL OF NEW ZEALAND (2012). Competencies for registered nurses Te whakarite i nga mahi tapuhi kia tiakina ai te haumaru a-iwi. Nursing Council of New Zealand, Wellington.
8. NEVILLE S (2008) Older people with delirium: Worthless and childlike. International Journal of Nursing Practice 14(6) 463-9.
9. HOLDEN J, JAYATHISSA S, YOUNG G (2008). Delirium among elderly general medical patients in a New Zealand hospital. Internal Medicine Journal 38(8) 629-34.
10. POTTER J, GEORGE J (2006). The prevention, diagnosis and management of delirium in older people: concise guidelines. Clinical Medicine 6(3):303-8.
11. AHMED S, LEURENT B, SAMPSON E (2014). Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age and Ageing 43(3) 326-33.
12. VANCOUVER ISLAND HEALTH AUTHORITY (2006). Delirium in the older person: A medical emergency [Internet]. Victoria, British Columbia, Vancouver Island Health Authority [updated 2014; cited 2014]. Available from: www.viha.ca/NR/rdonlyres/4DC32399-96E8-401B-9AAB-126BDD8A3512/0/delirium2_09.pdf
13. HOLROYD-LEDUC J, KHANDWALA F, SINK K (2010). How can delirium best be prevented and managed in older patients in hospital? Canadian Medical Association Journal 182(5) 465-70.
14. NICE GUIDELINES (2010) Delirium: diagnosis, prevention and management (CG103) Available at: www.nice.org.uk/guidance/CG103
15. O’MALLEY G, LEONARD M, MEAGHER D, O’KEEFFE S (2008). The delirium experience: a review. Journal of psychosomatic research 65(3) 223-8.
16. BÉLANGER L, DUCHARME F (2011). Patients’ and nurses’ experiences of delirium: a review of qualitative studies. Nursing in critical care 16(6):303-15.
17. PRETTO M, SPIRIG R, MILISEN K, DEGEEST S, REGAZZONI P, HASEMANN W (2009). Effects of an interdisciplinary nurse-led delirium prevention and management program (DPMP) on nursing workload: a pilot study. International journal of nursing studies 46(6):804-12.
18. INOUYE S, FOREMAN M, MION L, KATZ K, COONEY, J (2001). Nurses recognition of delirium and its symptoms: Comparison of nurse and researcher ratings. Archives of Internal Medicine 161(20):2467-73.
19. MICHAUD L, BÜLA C, BERNEY A, CAMUS V, VOELLINGER R, STIEFEL F, ET AL (2007). Delirium: Guidelines for general hospitals. Journal of Psychosomatic Research 62(3):371-83.
20. TROPEA J, SLEE J, BRAND C, GRAY L, SNELL T (2008). Clinical practice guidelines for the management of delirium in older people in Australia. Australasian journal on ageing 27(3):150-6.
21. GOVERNMENT OF WESTERN AUSTRALIA DOH (2008). Delirium Model of Care. In: Department of Health ACN, editor. Perth: Department of Health, Western Australia; 2008.
22. FONG T, TULEBAEV S, INOUYE S (2009). Delirium in elderly adults: diagnosis, prevention and treatment. Nature Reviews Neurology 5(4):210-20.
23. SENDELBACH S, GUTHRIE P, SCHOENFELDER D (2009). Acute confusion/delirium: identification, assessment, treatment and prevention. Journal of Gerontol Nursing 35(11):11-8.
24. MILLER C (2012). Miller’s nursing for wellness in older adults. Hunter S, editor. Sydney, Australia: Lippincott Williams & Wilkins; 2012.
25. DAY J, HIGGINS I, KOCH T (2008). Delirium and older people: what are the constraints to best practice in acute care? International journal of older people nursing 3(3) 170-7.
26. YOUNG J, INOUYE S (2007). Delirium in older people. BMJ334(7598) 842-6.
27. HOLROYD A, DAHLKE S, FEHR C, JUNG P, Hunter A (2009). Attitudes toward aging: implications for a caring profession. The Journal of Nursing Education 48(7) 374-80.
28. WHEELER M, CRENSHAW C, GUNN S. Incidence and Prevention of Delirium in Critical Care Patients. Critical Care Nursing Clinics of North America.
29. AMERICAN PSYCHOLOGICAL ASSOCIATION (2013). Diagnostic and statistical manual of mental disorders (5th ed) Washington, DC.
30. STEIS M, FICK D (2008). Are nurses recognizing delirium? A systematic review. Journal of gerontological nursing 34(9) 40-8.
31. LEMIENGRE J, NELIS T, JOOSTEN E, BRAES T & ET AL (2006). Detection of Delirium by Bedside Nurses Using the Confusion Assessment Method. Journal of the American Geriatrics Society 54(4) 685-9.
32. IRVING K & FOREMAN M (2006). Delirium, nursing practice and the future. International journal of older people nursing 1(2) 121-7.
33. CHAN P(2011). Clarifying the confusion about confusion: Current practices in managing geriatric delirium. British Columbia Medical Journal 53(8) 409-15.
34. BALAS M, RICE M, CHAPERON C, SMITH H & ET AL (2012). Management of Delirium in Critically Ill Older Adults. Critical Care Nurse 32(4) 15-26.
35. DAHLKE S &PHINNEY A (2008). Caring for hospitalized older adults at risk for delirium: the silent, unspoken piece of nursing practice. Journal of gerontological nursing 34(6) 41-7.
36. FICK D & MION L (2008). Delirium superimposed on dementia. American Journal of Nursing 108(1) 52-60.
37. ROSENBLOOM D & FICK D (2014). Nurse/family caregiver intervention for delirium increases delirium knowledge and improves attitudes toward partnership. Geriatric Nursing 35(3) 175-81.
THE HOUR OF POWER:
Reading the article and undertaking this Think delirium learning activity is equivalent to 60 minutes of professional development. Discuss all your answers with a peer.























